Hepatitis, a liver inflammation that affects millions globally, often leaves people feeling overwhelmed. From understanding its complex nature to finding effective treatments and preventative measures—it’s no small feat.
Did you know? Hepatitis A is not treated with specific medicines but rather focuses on supportive care and prevention strategies. This article aims to demystify hepatitis by breaking down its types, transmission routes, symptoms, and much more in a way that’s easy to grasp.
We promise insights and practical advice to navigate this health challenge confidently.
Keep reading—knowledge is power.
Key Takeaways
- Hepatitis is an inflammation of the liver with several types, including A, B, and C. Type A spreads through contaminated food or water and does not have specific medicines for treatment.
- Vaccinations are crucial for preventing hepatitis A and B. Safe hygiene practices and safe sex using barrier methods can help avoid catching or spreading hepatitis.
- For hepatitis B and C, which may lead to chronic conditions, antiviral medications can effectively fight the infection. Regular doctor visits are important for managing the disease.
- Liver damage from chronic hepatitis can result in serious conditions like cirrhosis or liver cancer over time. Preventative measures and early treatment are key to maintaining good liver health.
- Adopting healthy lifestyle changes such as avoiding alcohol, eating a balanced diet, and getting regular exercise supports liver recovery from hepatitis.
What is Hepatitis?
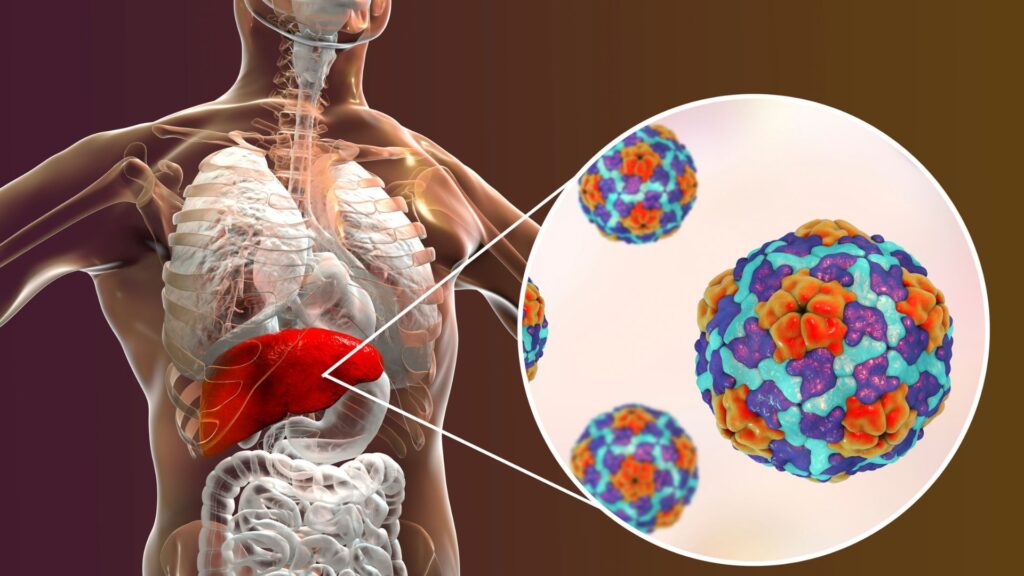
Hepatitis is an inflammation of the liver, often caused by viral infections. There are several types, including A, B, and C, each with different causes and effects on your health.
Definition
Hepatitis is a contagious liver infection. The World Health Organization provides detailed insights on its causes, mainly pointing to viruses as the culprits behind varying forms of hepatitis, including types A, B, C and others.
For example, Hepatitis A thrives in conditions where it can spread through contaminated food or water, leading to an acute illness that affects liver function temporarily.
Understanding this condition underscores the importance of prevention and immunization—especially since there are no specific medicines for treating hepatitis A. With heavy alcohol use, certain medications, toxins, and other medical conditions also posing risks for developing different types of hepatitis beyond viral infections alone; public health measures become crucial.
Liver health hinges not just on treatment but significantly on preventative care to guard against such infectious diseases.
Types (A, B, C, etc.)
Hepatitis is a serious liver infection caused by viruses. Each type, from A to C and beyond, affects the liver in different ways.
- Hepatitis A: This type leads to an acute, short-term infection primarily transmitted through eating contaminated food or drinking contaminated water. It’s highly contagious but usually resolves on its own with supportive treatment. Vaccination plays a key role in prevention, given there are no specific medicines for treating it.
- Hepatitis B: Transmitted through contact with infectious body fluids like blood, semen, or vaginal secretions, this type can lead to both acute and chronic infections. Chronic hepatitis B can cause severe liver damage leading to cirrhosis or liver cancer over time. Vaccinations are available and recommended for hepatitis B prevention.
- Hepatitis C: Mostly spread through direct contact with infected blood and occasionally through sexual contact, hepatitis C often transitions into a chronic condition without noticeable symptoms at first. Chronic hepatitis C significantly raises the risk of developing liver cirrhosis or cancer. While there’s no vaccine against hepatitis C, antiviral medications can cure most cases.
Moving on to how hepatitis is transmitted further explores these risks and preventive measures…
How Hepatitis is Transmitted
Hepatitis spreads in several ways, catching many off guard. From eating contaminated food to sharing needles, this virus finds various pathways into new hosts.
Through contaminated food or water
Eating or drinking something that’s not clean can make you sick with hepatitis A. This virus spreads when food or water gets contaminated. Imagine someone who has the virus doesn’t wash their hands well after using the bathroom and then touches food.
If you eat that food, you could get hepatitis A too. It’s a common way people catch this contagious liver infection around the world.
Clean water and good hygiene are key to stopping hepatitis A from spreading. The disease is acute, meaning it comes on fast but doesn’t last long for most people. Thankfully, there is no specific medicine needed for most cases since the body fights off the infection on its own over time.
Prevention and immunization are important for dealing with hepatitis A.
Unprotected sex
Unprotected sex is a common way hepatitis spreads. Not using condoms or other barrier methods can expose individuals to the virus. Hepatitis B and C, in particular, can easily pass between partners through bodily fluids.
This kind of transmission puts people at risk for serious liver problems later on.
This risk highlights the importance of safe sex practices. Encouraging conversations about sexual health and hepatitis vaccination plays a key role in prevention efforts. Sharing knowledge helps protect communities from outbreaks linked to sexual contact.
Next, we explore how sharing needles also contributes to the spread of hepatitis.
Sharing needles
Moving from the risks associated with unprotected sex, it’s crucial to highlight another common way hepatitis spreads: sharing needles. This practice poses a significant risk for transmitting not just hepatitis B and C but also other infectious diseases.
Using the same needle or syringe as someone else can directly introduce infected blood into your bloodstream. Unlike hepatitis A, which doesn’t have specific medicines for treatment and focuses on prevention and immunization, both hepatitis B and C can lead to more severe health complications if not treated properly.
The act of sharing needles is particularly dangerous because it bypasses most natural body defenses against pathogens, allowing direct access to the bloodstream. For those infected by shared needle use, treatments are available but they require early diagnosis and proper medical care.
The emphasis on public health efforts is to educate about safe practices including using new, sterile needles for each injection – a simple yet effective precaution that significantly reduces the risk of contracting liver infections like hepatitis.
These measures are essential parts of broader strategies aimed at preventing liver disease among communities at risk.
Symptoms of Hepatitis
If you feel unusually tired or notice a yellowing of your skin, these could be signs of hepatitis. Nausea and vomiting are also common symptoms to watch out for.
Fatigue
Fatigue is a common symptom of hepatitis, signaling that the liver isn’t working well. It means feeling very tired all the time, even if you rest. Your body fights hard against the hepatitis virus, which can make you feel worn out.
Since there are no specific medicines for treating hepatitis A and the disease is usually short-term, managing fatigue involves supportive care.
People with hepatitis often need to adjust their daily activities to cope with energy lows. Eating healthy foods, staying hydrated, and getting enough sleep can help manage this tiredness.
The right balance of activity and rest is key. Keep in mind that everyone’s experience with fatigue is different – listening to your body’s needs helps in dealing with this challenging symptom effectively.
Nausea/vomiting
Moving from fatigue, nausea and vomiting are also common symptoms of hepatitis. They occur as the body tries to rid itself of the virus. Eating or even thinking about food can make these feelings worse.
People with hepatitis may vomit because their liver struggles to process toxins normally.
Kids and adults alike might experience these discomforts during the early stages of hepatitis. Staying hydrated helps manage nausea and prevents dehydration from vomiting. Drinking clear fluids like water or ginger tea can ease the stomach.
It’s a direct way your body signals that something is wrong with liver function, urging you to seek medical advice for diagnosis and hepatitis treatment options available.
Jaundice
Jaundice is a common symptom of hepatitis, signaling liver trouble. The skin and whites of the eyes turn yellow due to high levels of bilirubin, a pigment in bile. This condition suggests that the liver isn’t processing substances as it should.
People with hepatitis may notice this sign along with other symptoms. It’s crucial for those experiencing jaundice to seek medical advice promptly for proper diagnosis and treatment.
The presence of jaundice often points to acute liver infection such as hepatitis A, which causes short-term infection but can have serious effects on liver function if not addressed.
Since there are no specific medicines for treating hepatitis A directly, managing symptoms like jaundice becomes part of supportive care aimed at helping the liver recover. Preventing hepatitis through vaccination and safe hygiene practices is key in avoiding complications like jaundice that signal deeper health issues.
Diagnosis and Treatment
Finding out you have hepatitis and getting the right treatment starts with a simple blood test—learn how to manage the disease and regain control of your liver health.
Blood tests
Doctors use blood tests to find out if you have hepatitis. These tests check for signs of the virus in your blood and show how well your liver is working. They’re a key part of diagnosing liver infections like hepatitis A, B, and C.
Blood samples give experts important clues about what’s happening inside your body.
Medics may also measure substances in your blood that signal liver inflammation or damage. This helps them understand the type of hepatitis you might have and how serious it is. The results guide doctors in choosing the best treatment plan for each person’s needs.
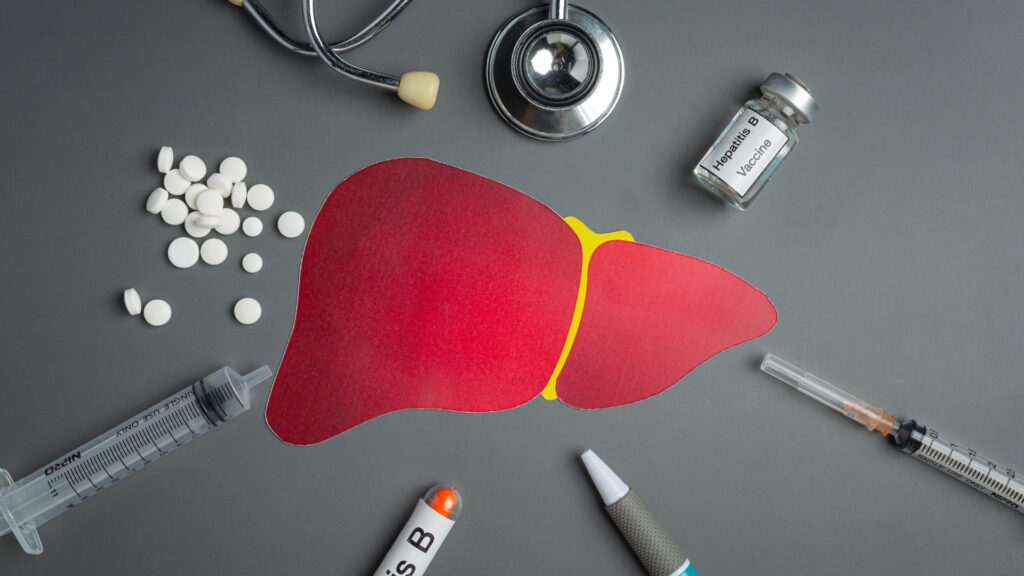
Medications
For hepatitis A, no specific medicines exist. The focus is on prevention through immunization and handling symptoms as they come. Since the disease is self-limiting, supportive care is key—this means staying hydrated, resting enough, and avoiding alcohol to help the liver recover.
Treatment for other types of hepatitis often includes antiviral drugs to fight the infection directly. These medicines can help reduce liver damage and slow down the virus. For severe cases, doctors might suggest more powerful options like interferon injections.
With careful management and regular doctor visits, many people with hepatitis can maintain their health and prevent serious liver problems.
Lifestyle changes
Moving from the discussion of medications, adopting healthier lifestyle habits plays a crucial role in managing hepatitis. This means cutting out heavy alcohol use since it can worsen liver conditions.
Individuals diagnosed with hepatitis need to be mindful of their body’s reactions to certain medications and toxins; avoiding these is key for liver health. Regular check-ups become part of life to monitor liver function and prevent severe complications like cirrhosis or liver cancer.
Eating a balanced diet rich in fruits, vegetables, and whole grains supports liver recovery. Drinking plenty of water helps flush toxins from the body, aiding in the healing process.
Engaging in moderate exercise strengthens the immune system which is vital in fighting off infections. Public health guidelines also suggest getting vaccinated against hepatitis A and B as a preventive measure.
These simple yet effective steps assist those recovering from hepatitis and act as preventative measures for healthy individuals aiming to maintain optimal liver health.
Long-Term Effects of Hepatitis
Living with hepatitis can lead to serious liver problems. Over time, it might cause liver failure or cancer.
Liver damage
Liver damage is a serious long-term effect of hepatitis. This condition can lead to scarring, known as cirrhosis, and may result in liver cancer if not addressed properly. Heavy alcohol use, certain medications, toxins, and underlying medical conditions are common culprits behind liver damage beyond just viral infections.
Preventing this type of liver harm involves understanding its causes such as hepatitis A which is highly contagious but preventable through vaccination. Without specific medicines for treating hepatitis A itself, focusing on prevention is crucial—emphasizing the importance of immunization and safe practices to maintain liver health.
Cirrhosis
Cirrhosis is a severe condition where the liver slowly deteriorates and malfunctions due to chronic injury. Scar tissue replaces healthy liver cells, blocking blood flow through the liver and slowing its processing functions.
This condition often stems from long-term effects of diseases such as hepatitis or from chronic alcohol abuse. Over time, it can lead to liver failure or cancer if not addressed.
Managing cirrhosis involves stopping the progression of liver damage. Measures include medication for hepatitis, avoiding alcohol, and maintaining a healthy diet to support liver health.
In advanced cases, a liver transplant may become necessary. Regular check-ups are crucial for monitoring liver function and managing complications effectively.
Liver cancer
After discussing cirrhosis, it’s crucial to shift our attention to liver cancer, a serious long-term effect of hepatitis. Liver cancer can develop when liver cells grow uncontrollably.
This usually happens after years of liver damage and inflammation. Hepatitis B and C are among the top causes of liver cancer worldwide, making them a significant public health issue.
Liver cancer is challenging because symptoms might not appear until the disease is advanced. People with a history of hepatitis or cirrhosis have a higher risk of developing this type of cancer.
Monitoring liver health and regular check-ups are vital for those at risk to catch any signs early.
Prevention through vaccination and leading a healthy lifestyle remains our best defense against hepatitis-induced liver cancer.
Prevention of Hepatitis
Stopping hepatitis starts with knowing how to avoid it. We can stay healthy by getting vaccines and following clean habits.
Vaccinations
Vaccinations play a crucial role in the prevention of hepatitis A. As there are no specific medicines for treating this infection, getting vaccinated is key to protection. The World Health Organization highlights immunization as an effective measure against the virus.
Hepatitis A vaccination can prevent the disease from taking hold by preparing the body’s immune system to fight it off.
For those at risk, including travelers to areas with high rates of hepatitis A, healthcare workers, and people with chronic liver diseases, vaccinations provide a shield against potential infection.
Public health experts recommend vaccination for children and adults alike to curb the spread of hepatitis A. This proactive approach saves lives and prevents long-term effects on the liver by stopping the virus before it starts.
Safe hygiene practices
Moving from vaccinations, practicing safe hygiene stands as another cornerstone in preventing hepatitis. Washing hands thoroughly with soap and water can significantly reduce the risk of contamination.
This simple act is especially crucial before eating or preparing food and after using the bathroom. Using alcohol-based hand sanitizers when soap and water are not available also helps keep germs at bay.
Keeping personal items personal prevents the spread of hepatitis. Items like toothbrushes, razors, and nail clippers should never be shared. These small tools can easily carry viruses from one person to another if used improperly.
Ensuring that food and water consumed are clean and safe further minimizes chances of catching hepatitis A, which often spreads through contaminated sources.
Safe sex
Safe sex is a crucial step in preventing the spread of hepatitis, especially types like hepatitis B and C, which can transmit through unprotected sexual contact. Using barriers such as condoms or dental dams every time you have sex reduces your risk of catching or spreading the virus.
It’s not just about protection—it’s also about maintaining healthy sexual relationships and ensuring liver health for both you and your partners.
Educating yourself and others on the importance of vaccinations can further shield against certain types of hepatitis. For instance, there are vaccines available for hepatitis A and B; getting these shots is an effective way to prevent these viruses from affecting your liver.
Always discuss with a healthcare provider to stay updated on immunizations, which serve as a defense mechanism for your body against these serious infections.
Conclusion
Hepatitis grabs our attention due to its impact on liver health, demanding a deeper understanding. Dr. Jordan Fields emerges as an expert in the field with over two decades dedicated to studying liver diseases, including hepatitis.
Graduating from a prestigious medical school and accumulating vast research experience, Dr. Fields has contributed significantly to our knowledge of viral infections affecting the liver.
Dr. Fields scrutinizes “Understanding Hepatitis: A Comprehensive Guide, Supplements, Medicines,” highlighting how it elucidates the complexity of hepatitis transmission and management.
He emphasizes that this resource accurately outlines preventive measures—like vaccinations—and lifestyle adjustments essential for mitigating disease spread and progression.
On safety and ethics, Dr. Fields commends the guide for adhering to scientific rigor and transparency about hepatitis’ nature and treatment options available currently. His insights affirm that providing clear information on certifications related to treatments ensures patients can make informed decisions regarding their care pathways.
Integrating knowledge from this comprehensive guide into daily life could be transformative for individuals at risk or those living with hepatitis, according to Dr. Fields. Regular screenings and adopting safe hygiene practices stand out among his top recommendations for utilizing these insights effectively in everyday scenarios.
In terms of benefits versus drawbacks, Dr. Fields acknowledges that while the guide serves as an invaluable tool for education on hepatitis prevention and treatment, reliance solely upon supplements without professional guidance could pose risks.
Thus, he advises weighing this option against conventional medical treatments under healthcare supervision.
Finally, Dr. Jordan Fields offers a strong endorsement of “Understanding Hepatitis: A Comprehensive Guide,” recognizing its contribution to informing public health strategies against viral hepatic infections effectively.
FAQs
1. What is Hepatitis and why should I understand it?
Hepatitis refers to an inflammation of the liver, often caused by a virus. Understanding this condition is crucial as it can lead to severe health complications if not properly managed or treated.
2. How can supplements and medicines help manage Hepatitis?
Certain supplements and medicines are designed to boost liver health, combat viral infections, or alleviate symptoms associated with Hepatitis. They play a vital role in managing the disease and enhancing the patient’s quality of life.
3. Are there different types of Hepatitis that require different treatments?
Yes indeed! There are five main types—A, B, C, D, E—each having unique causes and treatment protocols. It’s essential for individuals diagnosed with Hepatitis to follow their healthcare provider’s advice on appropriate medication or supplement regimen.
4. Is there a comprehensive guide available for understanding Hepatitis?
Absolutely! Comprehensive guides provide detailed explanations about the cause, symptoms, diagnosis methods, treatment options—including supplements and medicines—for each type of hepatitis; offering insights into living a healthy lifestyle despite being diagnosed with this condition.
General Facts
- Hepatitis A is a contagious liver infection caused by a virus.
- There are no specific medicines for treating hepatitis A.
- Prevention and immunization are important for hepatitis A.
- Heavy alcohol use, certain medications, toxins, and medical conditions can cause hepatitis.
- Hepatitis A is most often caused by a virus.
- Hepatitis A causes an acute, or short-term, infection.
- The disease is usually self-limiting and treatment and management are supportive.
- Hepatitis A spreads in different ways and can cause mild to serious effects on the liver.
- The World Health Organization provides key facts, transmission, who is at risk, treatment, prevention, and immunization for hepatitis A.
- It is important to learn how the disease spreads and what can be done to prevent or treat hepatitis A.











