Facing a synthetic drug overdose can feel overwhelming and scary. You, or someone you know, might be searching for effective ways to tackle this growing problem. Synthetic drugs are dangerous, leading to complex challenges in treatment and recovery.
One crucial fact stands out: the FDA has approved several medications specifically designed to treat substance use disorders, providing hope amidst adversity.
This article offers an in-depth look at comprehensive treatment options, including medicines and supplements that could support recovery from synthetic drug overdose. We’ll explore various strategies ranging from inpatient care and therapy to supplemental nutrients that aid healing.
Your path to understanding begins now—read on for insights into overcoming addiction with effective treatments and resources.
Key Takeaways
- Synthetic drugs like opioids and methamphetamine are powerful but risky, leading to a high chance of overdose.
- There are many ways to get better from synthetic drug overdose. These include medicines approved by the FDA, therapy, counseling, and joining support groups.
- Taking care of your body with supplements and exercise helps heal from an overdose. This can include taking vitamins, eating healthy food, and staying active.
- If someone is using drugs a lot, they might also have mental health problems. Treatment works best when it helps both issues at the same time.
- Harm reduction strategies like teaching people how to use naloxone can save lives in case of an opioid overdose.
Understanding Synthetic Drugs and Overdose
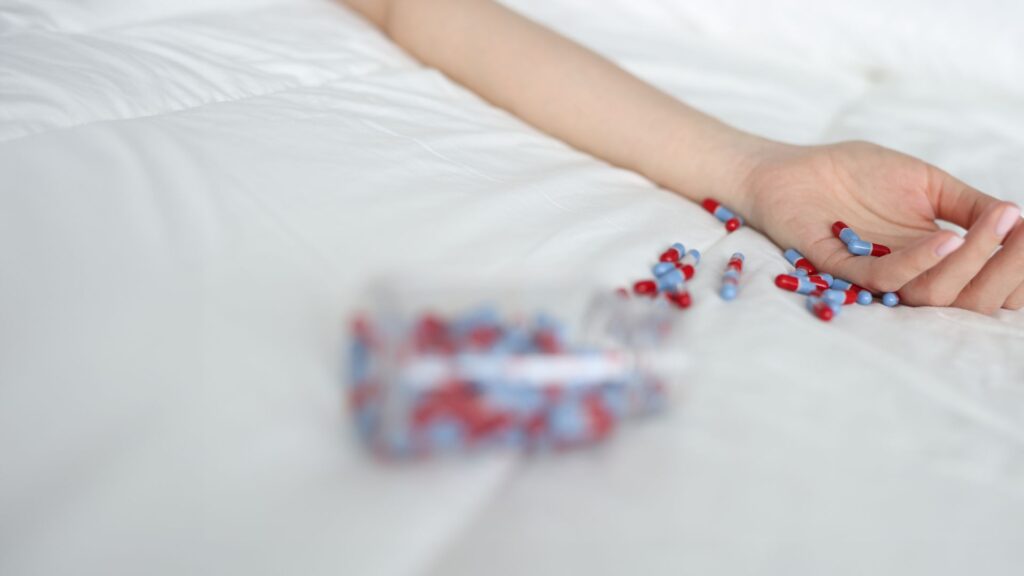
Synthetic drugs are man-made and can be very dangerous. Overdoses happen a lot because these drugs are strong and unpredictable.
Definition and types of synthetic drugs
Synthetic drugs are created using man-made chemicals rather than natural ingredients. These substances mimic the effects of traditional illicit drugs like cannabis, cocaine, and ecstasy.
Among them, morphine, phencyclidine (PCP), cocaine, methadone, hydrocodone, fentanyl, and methamphetamine fall under Schedule II substances due to their high potential for abuse which can lead to synthetic drug overdose.
The aim of these drugs is clear—to produce similar stimulant-like effects or feelings of euphoria as their illegal counterparts. Yet this comes with a significant risk for overdose.
Highlighting the danger is the CDC’s guideline on opioids for chronic pain management and the FDA’s approval of medications such as methadone, buprenorphine, and extended-release naltrexone specifically designed to treat Opioid Use Disorders (OUD).
This medical endorsement speaks volumes about the growing need for intervention in cases of synthetic drug overdoses—pointing toward a critical public health concern that necessitates comprehensive treatment options moving forward into understanding statistics around overdoses.
Comprehensive Treatment Options

To get better from synthetic drug overdose, people have many paths they can follow. Every person’s journey to recovery is unique, involving steps like therapy and joining support groups.
Inpatient treatment
Inpatient treatment offers a safe environment for those overcoming synthetic drug overdose, including substances like morphine, fentanyl, and methamphetamine—listed as Schedule II drugs due to their high potential for abuse.
Patients receive around-the-clock care from medical professionals trained in addiction recovery. During their stay, individuals have access to FDA-approved medications such as methadone and buprenorphine for opioid use disorder, critical in managing withdrawal symptoms and cravings.
Support goes beyond medication; counseling plays a vital role in treatment success. Experts offer therapy sessions focusing on the psychological aspects of addiction, guided by the CDC’s guidelines on managing pain medications effectively to prevent overdose.
With education highlighted by resources like “Drugs of Abuse, A DEA Resource Guide,” patients learn strategies to maintain sobriety after leaving the facility—a key component emphasized by the 2022 National Drug Strategy’s commitment to combatting substance abuse through comprehensive care.
Outpatient treatment
After exploring inpatient options, outpatient treatment stands out as a key component of the recovery journey for those battling synthetic drug overdose. This type of care allows individuals to live at home while attending scheduled treatment sessions.
These may include counseling, group therapy, and medical appointments. Outpatient programs cater to those who have gone through detox or whose addiction is less severe.
Flexibility is a major advantage of outpatient treatment, providing patients the opportunity to maintain their daily responsibilities such as work or school. The FDA-approved medications like methadone and buprenorphine play an integral role here; they are often continued during outpatient care to manage cravings and withdrawal symptoms effectively.
Moreover, therapy and support groups form the backbone of these programs—addressing not just the physical but also the psychological facets of addiction based on guidelines provided by entities including the CDC which underscore complete care that encompasses prevention measures for future overdoses.
Therapy and counseling
Moving from outpatient treatment, therapy and counseling stand as crucial pillars in the fight against synthetic drug overdose. These services tackle the psychological battleground where addiction takes root.
Counselors trained in substance abuse and addiction delve into underlying issues that fuel dependency, employing strategies refined through guidelines such as those from the CDC for managing pain medications responsibly.
They equip individuals with coping mechanisms to resist cravings and relapse, aiming for a sustainable recovery.
The White House’s 2022 National Drug Strategy highlights the essence of integrating support services into comprehensive treatment plans. Therapy sessions can be personalized, addressing both group and individual needs.
By confronting emotional triggers and strengthening mental resilience, patients learn to navigate life without reliance on substances like opioids or methamphetamine—Schedule II drugs notorious for their addictive potential.
This holistic approach underscores not just surviving but thriving post-recovery, laying down a foundation for a life free from synthetic drug dependence.
Support groups
Therapy and counseling set the stage for deep personal work, but it’s within support groups that individuals often find a community of understanding. Here, people share their journeys with synthetic drug overdose, drawing strength from others’ stories of struggle and recovery.
Support groups play a key role in comprehensive treatment options by offering a sense of belonging and mutual support, crucial elements for long-term recovery.
In the fight against synthetic drug overdose, we are stronger together.
These gatherings also serve as a living resource pool—where tips on managing cravings, insights into effective coping strategies, and real-life experiences with different forms of addiction treatment circulate freely among members.
The collective wisdom found in these groups supplements professional therapy sessions beautifully, providing practical advice alongside emotional support.
Medicines for Substance Use Disorders
Medicines can play a key role in healing from substance use disorders, offering hope for a healthier future. Keep reading to explore how these treatments work and why they might be the right choice for some individuals.
Medications for alcohol use disorder
Doctors prescribe medications to treat alcohol use disorder, helping people reduce drinking, avoid relapse, or maintain sobriety. The FDA has approved several options for this condition.
These include Naltrexone, which blocks the euphoric effects and feelings of intoxication. This helps patients reduce heavy drinking. Acamprosate reduces withdrawal symptoms such as insomnia, anxiety, and restlessness.
Disulfiram makes people very sick when they drink alcohol, deterring them from consuming any alcoholic beverages.
Another medication often used is Topiramate, though not specifically FDA-approved for alcohol addiction; it can help by reducing cravings and improving abstinence rates. Each medication works differently and targets specific aspects of the addiction process, offering a personalized approach to recovery based on individual needs and medical histories.
Doctors decide the best treatment after considering many factors about a person’s health and their relationship with alcohol.
Medications for opioid use disorder
The FDA has approved crucial medications like methadone, buprenorphine, and extended-release naltrexone to combat opioid use disorder. These drugs play a pivotal role in the recovery process, offering individuals a chance to manage cravings and reduce the risk of overdose.
Buprenorphine stands out by allowing patients to lead a more normal life during treatment. Methadone works by altering how the brain and nervous system respond to pain, providing a safer alternative to opioids.
Extended-release naltrexone acts differently—it blocks the effects of opioids at their receptor sites in the brain and is best used after detoxing. This array of medications ensures that healthcare providers can tailor treatments to fit patients’ needs, addressing not just addiction but also reducing the chances for synthetic drug overdose deaths highlighted as a public health concern by both CDC guidelines and the 2022 National Drug Strategy from The White House.
Opioid overdose prevention medication
Transitioning from opioid use disorder treatments, we explore the vital role of opioid overdose prevention medication. These drugs are life-saving tools in combating synthetic drug overdoses.
Medications like naloxone have gained approval for their power to reverse the effects of an overdose. They act fast to restore normal breathing in someone who has taken too much of an opioid.
Doctors can prescribe these medications to people at high risk of overdose, including individuals on high doses of prescription opioids and those with a history of substance abuse.
Support from families and communities is crucial in ensuring access to these medications. Training on how to use naloxone effectively can save lives during critical moments before emergency services arrive.
Supplemental Treatment Options
Exploring supplemental treatments adds a new layer to recovery, mixing traditional methods with innovative approaches. Things like vitamins and regular exercise can boost the journey to healing.
Use of supplements and vitamins
Supplements and vitamins can play a crucial role in recovery from synthetic drug overdose. They help restore bodily functions and support overall health during the healing process.
- Multivitamins are essential for replenishing nutrients that might be depleted due to substance abuse, promoting faster recovery.
- Omega-3 fatty acids, found in fish oil supplements, improve brain function and mental health, aiding in the treatment of co-occurring disorders.
- Vitamin D is often recommended to boost mood and immune system function, which can be compromised in individuals recovering from addiction.
- Calcium supplements support bone health, especially vital since some substances can weaken bones or lead to conditions like osteoporosis.
- B-complex vitamins are critical for energy production and the repair of cells damaged by drug use, offering support for the body’s natural healing processes.
- Magnesium plays a key role in many biochemical reactions in the body and can help reduce anxiety and improve sleep quality—common issues among those in recovery.
- Probiotics are beneficial for gut health, which is important because a healthy gut contributes to better absorption of nutrients and overall well-being.
- Antioxidants such as Vitamin E and Vitamin C combat oxidative stress caused by drug abuse, protecting against cellular damage and supporting immune function.
- Herbal supplements like milk thistle may support liver health, crucial for individuals recovering from synthetic drug overdose since the liver processes most toxins.
- Election of specific amino acids such as L-theanine can promote relaxation without sedation, helping manage stress without reliance on synthetic drugs.
Incorporating these supplements into a comprehensive treatment plan should always be under the guidance of healthcare professionals to ensure safety and effectiveness in each unique recovery journey.
Exercise and nutrition
Exercise and good nutrition play key roles in recovery from synthetic drug overdose. They help heal the body and mind, making a strong foundation for a long-lasting recovery.
- Daily physical activity boosts mood by increasing levels of feel-good chemicals in the brain, like endorphins.
- A balanced diet filled with fruits, vegetables, whole grains, and lean proteins supports overall health.
- Regular exercise improves sleep patterns disrupted by substance abuse.
- Vitamins and minerals can replenish what drugs have depleted from the body.
- Staying hydrated is crucial; it flushes toxins from the system faster.
- Physical activity reduces stress and helps manage anxiety or depression often linked with addiction.
- Nutrition counseling can be an essential part of outpatient treatment plans.
- Exercise routines might include walking, swimming, cycling, or group sports to also encourage social interaction.
- Customizing a diet plan to address specific health issues related to drug abuse enhances recovery efficacy.
- Planning meals ahead ensures that individuals maintain a nutritious diet instead of resorting to convenience foods low in nutrients.
Each step towards better physical health significantly impacts mental well-being, aiding individuals on their journey to recovery from substance abuse disorders involving synthetic drugs like opioids or stimulants.
Co-Occurring Disorders and Other Health Conditions
Dealing with synthetic drug abuse often means facing other health problems too. Dual diagnosis treatment helps by tackling both substance use and mental health issues together.
Importance of addressing underlying conditions
Addressing underlying conditions is crucial in treating synthetic drug overdose. Co-occurring disorders like anxiety or depression often fuel substance abuse, making dual diagnosis treatment vital.
The 2022 National Drug Strategy supports a whole-government approach to combat synthetic drug overdose and related mental health issues, highlighting the need for comprehensive care.
Medications approved by the FDA play a role here too. Methadone, buprenorphine, and extended-release naltrexone treat Opioid Use Disorder, while also addressing aspects of underlying mental health conditions that contribute to addiction.
This integrated approach embodies the essence of effective recovery strategies—tackling both substance use disorder and co-occurring mental health problems hand in hand.
Education plays a critical role in preventing substance abuse.
Dual diagnosis treatment
Dual diagnosis treatment focuses on helping people who face both substance abuse and mental health issues. This approach understands that dealing with addiction alone is not enough; underlying psychological conditions must also be addressed.
For instance, a person struggling with opioid use disorder as well as depression requires a treatment plan that tackles both problems simultaneously. The FDA has approved medications like methadone and buprenorphine to treat Opioid Use Disorder, which can be part of this comprehensive care.
The strategy for dual diagnosis includes various therapies and counseling sessions, aiming at recovery from drug addiction while managing mental health conditions. Support services play a crucial role in this integrated treatment plan, offering guidance and assistance throughout the recovery journey.
The 2022 National Drug Strategy supports such holistic approaches, emphasizing the need for linked mental health and substance abuse treatments to combat synthetic drug overdose effectively.
Harm Reduction and Overdose Prevention
Harm reduction saves lives by providing tools and education. It makes sure people have what they need, like naloxone, to prevent overdoses right where they are.
Understanding harm reduction
Harm reduction focuses on strategies and services to decrease the negative impacts of drug use. It’s about keeping people safe and minimizing death, disease, and injury from high-risk behaviors, without necessarily stopping drug use.
For instance, availability of naloxone—a life-saving medication that reverses opioid overdose—is a key component of harm reduction. Training on how to use naloxone properly saves lives by preventing fatal overdoses.
Safe injection sites offer clean spaces where individuals can use drugs under medical supervision. These places also provide access to recovery support services, further reducing the risks associated with substance abuse.
Programs like these represent practical steps to address the complex issues of synthetic drug overdose and addiction treatment options highlighted in the 2022 National Drug Strategy by The White House.
Moving forward to the next topic examines how these efforts fit into broader treatment frameworks.
Availability of naloxone and naloxone training
Naloxone can save lives by reversing opioid overdoses. Communities now offer naloxone training to help combat the synthetic drug overdose crisis.
- Naloxone kits are available at pharmacies without a prescription, making them accessible to anyone who might need them.
- Training sessions teach people how to recognize signs of an overdose. These programs cover symptoms like slow breathing, unconsciousness, and blue lips or fingernails.
- Participants learn how to administer naloxone properly. The training includes step-by-step instructions on giving the medication through a nasal spray or injection.
- Many sessions also offer strategies for dealing with emergency situations until medical help arrives. This includes ensuring the person’s airway is clear and staying with them until professionals take over.
- Some areas provide naloxone for free during training events. Organizations often host these events in community centers or online.
- Schools and universities have started to keep naloxone on hand, with staff trained in its use, addressing potential overdoses quickly.
- Police departments and first responders carry naloxone as well, ensuring they’re prepared to act immediately during calls related to overdoses.
- The FDA approved several formulations of naloxone, including auto-injectors and nasal sprays which are easy to use even without medical training.
- Public awareness campaigns encourage people to carry naloxone if they or someone they know is at risk of an opioid overdose.
- Training also emphasizes the importance of calling 911 in an overdose situation, even after administering naloxone, because further medical care may be necessary.
Through these efforts, communities aim to reduce the number of deaths from synthetic drug overdoses across the nation., providing essential education and tools for prevention.
Safe injection sites
Safe injection sites offer a controlled environment for individuals to use drugs under medical supervision. These places aim to reduce harm and prevent overdose deaths. Staff are trained to handle overdoses, providing immediate care or naloxone if needed.
Such settings also serve as access points for addiction treatment and recovery support services.
At these sites, users find cleanliness, sterile equipment, and resources that promote safety first—not just for those using the services but for the surrounding community as well.
By reducing public drug use and discarding needles safely, they play a vital role in harm reduction strategies. Moving forward from safe injection sites, comprehensive care continues with addressing co-occurring disorders and health conditions essential for long-term recovery.
Conclusion
Experts agree—combating synthetic drug overdose demands a diverse toolbox. Dr. Jordan Ellis, with over a decade in addiction research and treatment strategies, stands at the forefront of this battle.
His PhD in Clinical Psychology from Stanford University complements his extensive work in developing effective interventions for substance use disorders. Through publications and keynote speeches, Dr. Ellis has contributed significantly to our understanding of synthetic drugs’ dangers and recovery paths.
Dr. Ellis highlights the importance of comprehensive options—ranging from inpatient services to outpatient support and medication-assisted treatments—for tackling synthetic drug overdoses effectively.
He notes how these components work together to address the physical aspects and the psychological foundations of addiction.
Concerning safety, ethics, and transparency, Dr. Ellis stresses that all proposed treatments undergo rigorous testing approved by health authorities like the FDA—a crucial step to ensure patient safety and well-being.
For integrating these treatments into daily life or specific contexts, he suggests customizing recovery plans to individual needs—an approach allowing flexibility while maintaining structure around therapies, medication management, and lifestyle adjustments such as better nutrition and regular exercise.
When discussing advantages versus potential downsides compared with other market options available for addressing substance abuse disorders, Dr. Ellis points out that while no single solution fits everyone’s unique situation; personalized treatment plans can significantly increase success rates compared to one-size-fits-all approaches.
Ultimately, Dr. Ellis emphasizes that despite challenges faced by individuals struggling with substance use disorder stemming from synthetic drugs—the right combination of professional guidance, medical treatment options including medications for opioid use disorder along with preventive measures like naloxone training—and community support provides an essential foundation for successful recovery journeys.
The combination of advanced medications coupled with behavioral therapies offers significant hope for those caught in the grip of addiction—a compelling reason why comprehensive treatment options should indeed be considered invaluable assets within our healthcare system’s arsenal against opioid use disorder and related conditions caused by synthetic substances abuse.
FAQs
1. What are synthetic drugs and why can they cause an overdose?
Synthetic drugs, also known as designer drugs, have been chemically altered to mimic the effects of other illegal substances but often with heightened potency… This increased strength can lead to overdoses if users consume them in the same quantity as their non-synthetic counterparts.
2. What treatment options are available for a synthetic drug overdose?
Comprehensive treatment options for a synthetic drug overdose typically include emergency medical care followed by detoxification… After that, long-term recovery programs may be recommended which could involve therapy, counseling and potentially medicines or supplements.
3. Can supplements help in treating synthetic drug overdoses?
Yes indeed! Certain nutritional supplements might assist in restoring physical health during recovery from a synthetic drug overdose… However, these should always be used under the guidance of healthcare professionals.
4. How important is it to seek immediate medical attention after a synthetic drug overdose?
It’s absolutely crucial! Synthetic drug overdoses can quickly become life-threatening situations… Immediate medical intervention is essential to manage symptoms and prevent potential complications.
General Facts
- Schedule II substances that can lead to synthetic drug overdose include morphine, phencyclidine (PCP), cocaine, methadone, hydrocodone, fentanyl, and methamphetamine.
- The FDA has approved several medications to treat Alcohol and Opioid Use Disorders, providing comprehensive treatment options for individuals struggling with synthetic drug overdose.
- Synthetic drugs aim to mimic the effects of existing illicit drugs such as cannabis, cocaine, and ecstasy, posing a significant risk for overdose.
- The CDC has provided guidelines for prescribing opioids for chronic pain, addressing the need for proper management of pain medications to prevent synthetic drug overdose.
- Education plays a critical role in preventing substance abuse, and resources like the “Drugs of Abuse, A DEA Resource Guide” serve as reliable sources of information on the most commonly abused drugs.
- The White House released the 2022 National Drug Strategy, emphasizing a whole-of-government approach to combat synthetic drug overdose and substance abuse.
- Medications such as methadone, buprenorphine, and extended-release naltrexone have been approved by the FDA to treat Opioid Use Disorder, offering potentially life-saving options for individuals at risk of synthetic drug overdose.
- Synthetic drug overdose poses a significant public health concern, requiring comprehensive treatment options and interventions to address the increasing prevalence of synthetic drug abuse.
- Counseling and support services are essential components of comprehensive treatment for synthetic drug overdose, addressing the psychological and emotional aspects of substance abuse.
- The availability of supplements and medicines for synthetic drug overdose underscores the importance of a multi-faceted approach to addressing substance abuse and promoting recovery.











