Facing liver issues can be scary, especially when the cause is related to medication use. Drug-related cirrhosis, a serious condition characterized by scarring of the liver, worries many.
Here’s a fact: specific medications taken over a long period can lead to this type of liver damage.
This blog aims to shed light on drug-related cirrhosis—covering everything from symptoms and diagnosis to treatments with medications and supplements. We’ll also explore valuable self-care tips and prevention strategies.
Ready for guidance? Keep reading for insights that could make all the difference.
Key Takeaways
- Alcohol can damage your liver, so cutting down prevents more harm.
- Doctors use medicines like Ademetionine and Ursodeoxycholic Acid to help your liver work better.
- Healthy foods and exercises make you stronger against cirrhosis.
- Supplements such as Milk Thistle and Omega-3s keep your liver healthy.
- Regular check-ups with a doctor catch liver problems early.
Understanding Cirrhosis of the Liver
Understanding cirrhosis of the liver starts with knowing its effects on your body. This condition can change how your liver works and affects your health.
Identifying Causes and Risk Factors
Cirrhosis of the liver can stem from long-term use of certain medications. This connection highlights the importance of managing prescriptions carefully to avoid unnecessary harm to this vital organ.
Pharmacists play a key role in this process by ensuring that patients receive medications that don’t interact poorly with each other, leading to adverse side effects or toxicities.
With cirrhosis, prevention focuses on stopping further liver damage by selecting treatments suited to the patient’s overall health and known allergies.
The goals of treatment for cirrhosis are to prevent further liver damage and to manage symptoms and complications effectively.
Risk factors for drug-related cirrhosis include hepatitis, alcoholic liver disease, and nonalcoholic fatty liver disease. These conditions contribute significantly to liver inflammation and damage over time.
Addressing these risk factors through lifestyle changes like reducing alcohol consumption and ensuring proper medication use is crucial in preventing cirrhosis. Regular check-ups allow for early detection and management of potential liver issues before they develop into more severe problems.
Recognizing Symptoms and Complications
After highlighting the causes and risk factors associated with cirrhosis, we turn our attention to its symptoms and complications. Fatigue and itching are common signs that may signal liver damage due to cirrhosis.
Yet, these symptoms barely scratch the surface. Patients can experience a range of issues including edema (swelling in legs), ascites (fluid buildup in the abdomen), jaundice (yellowing of skin and eyes), weight loss, nausea, and more severe conditions like hepatic encephalopathy—confusion resulting from liver failure—and portal hypertension.
Each symptom points to the liver struggling to perform its essential functions.
As cirrhosis progresses, managing these complications becomes vital for maintaining quality of life. Nutritional supplements might be prescribed to address malnutrition and help prevent weak bones—a common concern among those with liver disease.
The right medications play a key role here; they’re chosen based on the patient’s overall health and any allergies they may have. Importantly, pharmacists ensure that medication management is optimized to avoid drug-drug interactions or adverse effects that could worsen liver condition.
Thus, identifying and understanding these symptoms is crucial for preventing further damage and handling the existing challenges efficiently through lifestyle changes alongside medical treatment.
Progression Stages of Cirrhosis
Cirrhosis develops through stages, from mild to severe. Each stage brings more health issues and indicates how far the liver damage has gone.
Steps for Diagnosis
Diagnosing drug-related cirrhosis involves a series of steps to understand the liver’s health and function. Doctors use a combination of medical history, physical exams, and specific tests.
- Medical History Review: A doctor starts by asking about your medication use, alcohol consumption, and family history of liver disease. This helps identify potential causes of liver damage.
- Physical Examination: During the exam, the doctor looks for signs of liver disease. These may include jaundice (yellowing of the skin and eyes), swelling in the legs and abdomen (edema and ascites), and enlarged veins seen through the skin.
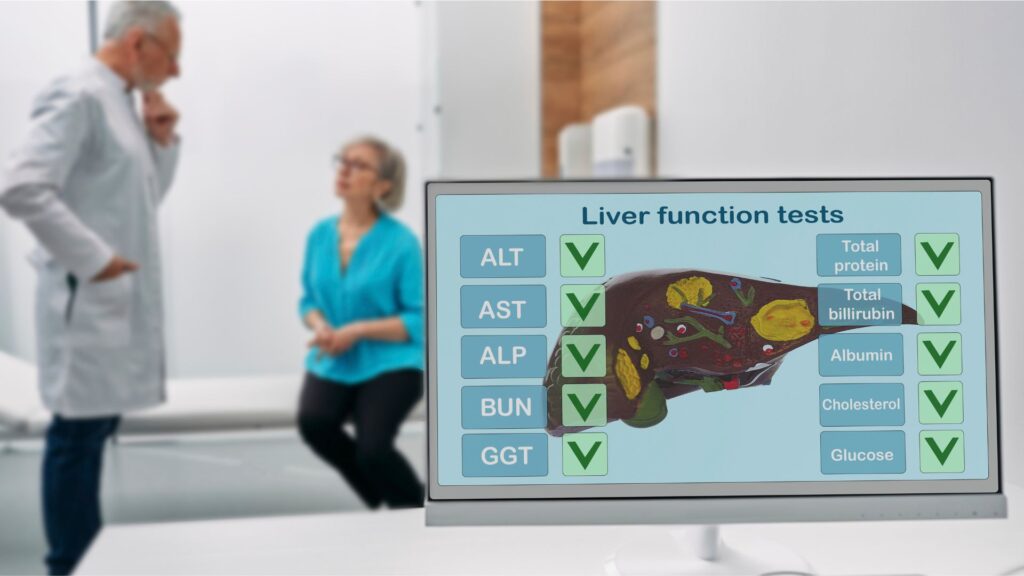
- Blood Tests: Several blood tests help assess liver function. These include tests for alanine transaminase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), bilirubin, and albumin levels.
- Imaging Tests: Ultrasound, CT scans, or MRIs can show liver scarring and other abnormalities. These imaging tools provide detailed pictures of the liver and surrounding tissues.
- Liver Biopsy: This is when a small sample of liver tissue is taken with a needle and examined under a microscope. It’s considered the most accurate test for diagnosing cirrhosis.
- Endoscopy: Doctors may use an endoscope to look for enlarged veins (varices) in your esophagus or stomach, which are common complications of cirrhosis.
- Elastography: This test measures the stiffness of your liver by ultrasound or magnetic resonance imaging (MRI) techniques. Increased stiffness can indicate fibrosis or scarring.
- Hepatic Function Panel Test: This comprehensive blood test provides information on various enzymes, proteins, and substances in your blood produced or processed by the liver.
- Reviewing Family Medical Histories: Knowing if close relatives have had liver disease might suggest a genetic predisposition to cirrhosis.
- Genetic Testing: In some cases, genetic tests may be recommended to identify inherited conditions that could contribute to liver damage.
Each step offers crucial insights into how well your liver works and helps guide treatment decisions specifically for you.
Available Treatment Options
Treatment options for cirrhosis focus on stopping further liver damage and managing symptoms effectively. Patients with drug-related cirrhosis often receive medications customized to their health needs, avoiding any that could cause adverse reactions or allergies.
Doctors may prescribe nutritional supplements to combat malnutrition and support overall liver health. These might include substances to strengthen bones, which can become weak due to the liver disease.
Lifestyle changes play a crucial role as well. People with cirrhosis are advised to alter their diet and incorporate regular exercise into their routines. Pharmacists contribute by optimizing medication regimens, ensuring there are no harmful drug-drug interactions or side effects that could worsen patient conditions.
The goal is always preventing more damage and easing complications like fatigue, itching, and swelling.
The National Institute of Diabetes and Digestive and Kidney Diseases highlights the importance of comprehensive treatment plans in managing cirrhosis caused by long-term medication use.
Moving forward from understanding treatment possibilities…
Effective Medications for Cirrhosis
Doctors often prescribe specific medicines for liver cirrhosis to help manage symptoms and slow the disease’s progression. These medications target various aspects of cirrhosis, supporting overall liver health and reducing complications.
Benefits of Ademetionine
Ademetionine plays a crucial role in managing cirrhosis, particularly in promoting liver health and function. By preventing further liver damage, this supplement aids patients in dealing with the challenges of hepatic cirrhosis.
The goal of using Ademetionine is to improve symptoms such as fatigue and itching, which are common among those suffering from liver disease. Its effectiveness is rooted in its ability to support liver regeneration and reduce inflammation.
Pharmacists recognize Ademetionine for its capacity to minimize adverse side effects and toxicities, especially important for cirrhosis patients who require careful medication management.
This supplement contributes to the prevention of malnutrition—a frequent complication associated with cirrhosis—and also assists in preserving muscle mass through better nutrient absorption.
With nutritional supplements like Ademetionine playing a vital part in treatment plans, patients often see an improvement in their overall quality of life while dealing with the challenges of drug-related liver disease.
Role of Ursodeoxycholic Acid
Ursodeoxycholic acid plays a crucial part in treating cirrhosis, especially when the liver’s bile flow gets slowed or blocked. This medicine helps move bile from your liver to your gut, which reduces damage and improves liver function.
Patients with drug-related cirrhosis often benefit from its use because it addresses one of the liver’s vital processes directly.
Doctors choose ursodeoxycholic acid based on a patient’s overall health and specific needs. Since preventing further liver damage is a key goal in managing cirrhosis, this medication fits well into comprehensive treatment plans for those facing symptoms like fatigue and itching due to impaired bile flow.
Its effectiveness makes it an essential option for many aiming to manage their condition better and avoid complications.
Use of Lactulose
Lactulose helps patients with liver cirrhosis by reducing the amount of ammonia in the blood. Doctors often prescribe this medication because high ammonia levels can lead to brain problems, like hepatic encephalopathy, a serious condition linked to liver disease.
Lactulose works by drawing ammonia from the blood into the colon where it’s removed from the body.
Taking lactulose regularly can greatly improve mental function and quality of life for those living with cirrhosis. It’s important for keeping the liver from working too hard and prevents more damage.
By managing symptoms effectively, lactulose plays a key role in treatment plans for liver health.
Lactulose: A vital tool in managing cirrhosis and safeguarding mental function.
Function of Propranolol
Propranolol works by slowing down the heart rate and decreasing blood pressure. This action helps reduce the pressure in the veins of the liver and stomach. For patients with cirrhosis, lower blood pressure in these areas can prevent complications like varices from bursting.
Varices are swollen veins that can bleed heavily if they burst, a severe risk for people with hepatic cirrhosis. By keeping blood flow at safer levels, propranolol plays a crucial role in managing portal hypertension, one of the complications mentioned under liver conditions such as hepatitis and alcoholic liver disease.
Turning to medication management pharmacists ensure that patients receive correct dosages of propranolol to avoid drug-drug interactions or adverse effects while treating cirrhosis.
Their goal aligns with preventing further liver damage and managing symptoms effectively—a key aspect highlighted for optimizing patient health amidst challenges posed by cirrhosis.
Next, let’s explore how recommended supplements support overall treatment strategies for this condition.
Recommended Supplements for Cirrhosis

Exploring the right supplements can significantly support liver health in cirrhosis patients—find out which ones are most effective for you.
Advantages of Milk Thistle
Milk thistle is a powerful supplement for those dealing with drug-related cirrhosis. It works by supporting the liver’s ability to regenerate healthy cells while fighting off harmful inflammation.
As cirrhosis can lead to malnutrition, incorporating milk thistle may also aid in preventing weak bones—a common complication among patients. This supplement stands out as it seeks to halt further liver damage and actively participates in the healing process.
Turning to milk thistle could be seen as a proactive step toward managing symptoms like fatigue and itching associated with cirrhosis. Given its potential to enhance nutritional status, it serves an important role alongside medications prescribed based on overall health and allergy considerations.
Pharmacists often recommend milk thistle within a treatment plan aimed at optimizing medication efficacy while minimizing risks of adverse side effects and toxicities in those living with hepatic conditions.
Importance of Vitamin D
Vitamin D plays a vital role for people with cirrhosis of the liver. It helps in preventing weak bones, which is crucial since nutritional supplements are often prescribed to address malnutrition associated with this condition.
Strong bones support overall health, making it easier for patients to stay active and manage symptoms more effectively.
Doctors recommend Vitamin D because it assists in calcium absorption—a key factor in bone strength. For those facing liver disease, maintaining good bone health becomes even more important.
This supplement supports physical well-being and contributes to the treatment goal of preventing further liver damage.
Benefits of Omega-3 Fatty Acids
After discussing the importance of Vitamin D for those dealing with cirrhosis, it’s key to highlight another crucial supplement—Omega-3 fatty acids. These nutrients play a significant role in maintaining overall liver health.
Omega-3s can help prevent inflammation and reduce the risk of chronic liver disease. For patients battling cirrhosis, this means potentially lessening further liver damage. Nutritional supplements like Omega-3 fatty acids are often prescribed to address malnutrition commonly seen in cirrhosis cases, aiding in bolstering the body’s defenses against complications.
These essential fats also contribute to stronger bones, combating weak bone issues that frequently accompany liver conditions. By integrating foods rich in Omega-3s or taking recommended supplements, individuals can proactively support their liver function and manage symptoms more effectively.
Engaging in lifestyle changes that include regular intake of Omega-3 fatty acids marks a positive step towards addressing malnutrition and enhancing overall well-being and quality of life for those affected by cirrhosis.
Self-Care Strategies for Cirrhosis
Taking care of yourself is key when dealing with cirrhosis. Learn to manage your symptoms and make healthy life changes for a better you.
Manage Symptoms like Fatigue, Itching, and Pain
Managing symptoms such as fatigue, itching, and pain is crucial for patients with drug-related cirrhosis. These strategies help improve quality of life and may prevent complications.
- Stay hydrated to minimize fatigue—drinking enough water can flush toxins from your body that contribute to tiredness.
- Apply moisturizers regularly to soothe itching skin caused by bile salt buildup under the skin.
- Engage in light exercise, like walking or swimming; it boosts energy levels and can reduce fatigue.
- Use over-the-counter antihistamines for severe itching; they block the action of histamine, which can cause itchiness.
- Consider acupuncture or massage therapy to manage pain and improve relaxation.
- Eat small, nutritious meals throughout the day to maintain energy and address malnutrition associated with cirrhosis.
- Avoid foods high in sodium that can worsen edema and ascites, contributing to discomfort and pain.
- Implement a bedtime routine that promotes restful sleep—being well-rested helps combat daytime fatigue.
- Consult your doctor about pain relievers; some are safer for liver health than others.
- Incorporate relaxation techniques such as deep breathing exercises or meditation to naturally reduce pain levels.
Each of these steps addresses specific symptoms caused by drug-related cirrhosis, aiming at a holistic approach to managing this condition’s effects on the body.
Implement Dietary Changes
Eating the right foods can help manage liver disease. Making dietary changes is a crucial step toward improving your health if you have cirrhosis.
- Cut down on salt to reduce swelling in your body. Too much salt can make your body hold extra water, leading to swelling in the legs and belly.
- Eat more fruits and vegetables. They are full of nutrients and antioxidants that support liver health.
- Limit fatty foods to help your liver. Foods high in fat can be harder for your liver to process.
- Increase high-fiber foods like whole grains. Fiber helps your digestive system work better.
- Choose lean protein sources such as chicken, fish, and legumes. Protein is essential, but it’s important to pick options that are easy on the liver.
- Stay hydrated by drinking plenty of water throughout the day. Water helps flush toxins from your body.
- Avoid alcohol completely since it can cause further liver damage.
- Control sugar and refined carbohydrates intake as they can lead to spikes in blood sugar levels, stressing the liver.
- Incorporate healthy fats like those found in avocados, nuts, and olive oil into your diet to support overall well-being without overburdening the liver.
- Take vitamin supplements if recommended by your doctor to address malnutrition often seen in cirrhosis patients and prevent weak bones.
Making these dietary changes plays a key role in managing symptoms of cirrhosis, preventing further liver damage, and supporting overall health improvements alongside medication management prescribed by healthcare professionals.
Incorporate Exercise
Exercise plays a vital role in managing cirrhosis. It helps improve liver function and overall well-being.
- Start with low-impact activities like walking or swimming to gently boost your energy levels without overstraining your body.
- Gradually increase the duration and intensity of your workouts as you build stamina, aiming for at least 30 minutes of moderate exercise most days of the week.
- Incorporate strength training exercises twice a week to maintain muscle mass, which can be affected by malnutrition in cirrhosis.
- Engage in flexibility and balance exercises such as yoga or Tai Chi to enhance physical function and reduce fall risk, especially important for those with portal hypertension or ascites which can impair balance.
- Always listen to your body—rest when tired and avoid pushing too hard, since fatigue is a common symptom of cirrhosis.
- Keep hydrated during exercises, especially important as cirrhosis can affect fluid balance within the body.
- Consult with a healthcare professional before starting any new exercise program, particularly if you have complications like hepatic encephalopathy or severe portal hypertension, to customize the regimen to your needs safely.
- Monitor for any signs of increased abdominal swelling or discomfort after exercising, which could indicate worsening ascites and require medical attention.
- Make exercise a regular part of your routine but be flexible—adjust activities based on how you feel each day.
- Consider joining a group class or finding an exercise buddy for motivation and support as you work towards improving your health through physical activity.
Incorporating these steps into daily life can help manage symptoms of cirrhosis effectively while contributing to improved liver health and quality of life.
Strategies to Prevent Cirrhosis
To keep your liver healthy and avoid cirrhosis, start by cutting down on alcohol and being careful with medicines. Regular check-ups help catch any liver issues early.
Reduce Alcohol Consumption
Cutting down on alcohol is key in preventing liver damage and managing cirrhosis. Alcohol can harm your liver, especially if you already have liver disease. By reducing how much you drink, you help your liver heal and stop more damage from happening.
It’s a simple step with big benefits for your health.
Limiting alcohol intake can significantly reduce the risk of developing cirrhosis, says experts from the National Institute of Diabetes and Digestive and Kidney Diseases. Making this change supports treatment goals like preventing further liver damage and dealing with symptoms such as fatigue and itching effectively.
Ensure Proper Medication Use
Using medications correctly is vital for people with cirrhosis. Since the liver processes most drugs, patients must work closely with their doctors to choose the right meds. This helps avoid harm to their already damaged liver.
For instance, pharmacists can guide on avoiding drug-drug interactions and minimizing side effects from medicines.
Patients should always tell their health care providers about all medicines they take, including over-the-counter ones and supplements. This step is crucial in preventing further liver damage and managing symptoms effectively.
With proper medication use, patients can aim to stop the progression of drug-related cirrhosis while keeping complications at bay.
Schedule Regular Check-Ups
Seeing your doctor for regular check-ups is key to preventing cirrhosis from getting worse. During these visits, doctors can catch early signs of liver damage or complications before they become serious.
They use blood tests and imaging studies to monitor liver health closely. This helps in adjusting treatments as needed and avoiding potential drug-drug interactions that pharmacists watch out for.
Doctors also take this time to manage symptoms like fatigue and itching, which are common in cirrhosis patients. By scheduling these appointments ahead of time, you ensure that your liver’s condition is continually assessed, allowing for timely interventions.
Next up: exploring how reducing alcohol consumption plays a crucial role in cirrhosis prevention.
Conclusion
Cirrhosis damages the liver, turning healthy tissues into scarred ones. This condition can sneak up on you, showing few symptoms at first but leading to severe health problems if untreated.
Fighting back involves knowing what medicines and supplements work best and making lifestyle changes that boost your overall well-being.
Dr. Elizabeth Torres stands out as an authority in treating liver diseases like cirrhosis. With over 20 years of experience, her background includes a specialization in hepatology, numerous publications on liver health, and groundbreaking research that has paved the way for innovative treatments.
Driven by passion, Dr. Torres commits to enhancing patient outcomes through comprehensive care strategies.
According to Dr. Torres, understanding the key components of managing cirrhosis—medication management, nutritional supplementation, and self-care—is crucial for effective treatment outcomes.
She stresses the importance of Ademetionine for its regenerative properties and Ursodeoxycholic Acid for reducing bile acid toxicity in cirrhotic patients. Lactulose helps manage potential brain complications while Propranolol prevents bleeding from enlarged veins in the esophagus.
Regarding safety and ethics in cirrhosis treatment, Dr. Torres values transparency above all else. Certifying trustworthiness through credentials, she argues for honest communication between healthcare providers and patients about potential medication side effects.
Implementing these treatments into daily life requires patience and adjustment. She advises incorporating Milk Thistle supplements progressively to assess tolerance levels. Similarly with exercise—a moderate approach specific to individual capacities ensures benefits without overwhelming a compromised liver.
Offering a balanced view, she notes while these medications excel at slowing disease progression, they cannot reverse existing liver damage. Comparatively speaking, several alternative therapies may offer palliative benefits, yet their efficacy often lacks solid scientific support.
Thus, choosing evidence-backed options remains paramount.
Ultimately, according to her, early intervention combined with proven therapeutic strategies enormously enhances quality of life even with serious conditions like drug-related cirrhosis.
Her endorsement rests firmly on treatments grounded in rigorous testing, underscoring their significant role alongside dietary adjustments and regular check-ups. Equal emphasis lies on both preventing further damage and alleviating present symptoms, making them invaluable resources for those contending with this challenging disease path.
FAQs
1. What are the symptoms of drug-related cirrhosis?
Symptoms of drug-related cirrhosis can vary greatly but often include fatigue, loss of appetite, yellowing skin or eyes (jaundice), and swelling in your legs or abdomen.
2. How is drug-related cirrhosis treated?
Treatment for this condition typically involves a comprehensive plan that may include medicines to reduce liver damage, dietary changes to support overall health, and potentially even surgery in severe cases.
3. Can supplements help manage drug-related cirrhosis?
Yes! Certain supplements might aid in managing the symptoms and slowing down the progression of this disease. However, it’s crucial to consult with a healthcare professional before starting any new supplement regimen.
4. Is there a guide I can follow for dealing with drug-related cirrhosis?
Absolutely! There are numerous resources available that provide detailed explanations on recognizing symptoms, understanding treatment options including medicines and supplements, as well as lifestyle modifications necessary for managing this condition effectively.
General Facts
- Cirrhosis of the liver can be caused by long-term use of certain medications.
- Symptoms of drug-related cirrhosis can include fatigue and itching.
- Nutritional supplements may be prescribed to address malnutrition associated with cirrhosis.
- Supplements can also help prevent weak bones in patients with cirrhosis.
- Several medications are available to treat cirrhosis, and the right one will be chosen based on the patient’s overall health and any allergies.
- Pharmacists can play a role in optimizing medications to prevent drug-drug interactions, adverse side effects, and toxicities in cirrhosis patients.
- The goals of treatment for cirrhosis are to prevent further liver damage and manage symptoms and complications.
- Lifestyle changes may also be used as part of the treatment for drug-related cirrhosis.
- A comprehensive guide covering causes, diagnosis, symptoms, treatment, and prevention of cirrhosis is available for patients and healthcare professionals.
- The National Institute of Diabetes and Digestive and Kidney Diseases offers information on treatments for cirrhosis due to long-term use of certain medications.
Source URLs
- WebMD – Understanding Cirrhosis: Basic Information
- Mayo Clinic – Cirrhosis Diagnosis and Treatment
- Healthline – Medication for Cirrhosis
- US Pharmacist – Drug Considerations in Cirrhosis
- American Liver Foundation – Cirrhosis Complications
- Drugs.com – Cirrhosis Health Guide
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Cirrhosis Treatment

