Finding the right cancer treatment can feel overwhelming. With so many options, it’s hard to know what will work best for you or your loved one. One promising area of research and treatment is gene therapy, an approach that targets cancer at its genetic roots. Gene therapy holds the power to revolutionize how we treat cancer, offering new hope where traditional treatments fall short.
One important fact about this topic is that the U.S. Food and Drug Administration has approved several gene therapy products for treating cancer and rare diseases. This means patients now have more options than ever before. In our guide, we will walk you through what gene therapy for cancer involves, including supplements and medicines that complement these advanced treatments. We’ll help make sense of complex terms and offer insight into how these therapies are changing lives.
Stay with us to learn more.
Key Takeaways
- Gene therapy corrects faulty genes causing cancer, using CRISPR and FDA-approved products to offer personalized treatment.
- Exploring new treatments like immune cell gene therapy and oncolytic virus therapy gives patients hope against tough diseases.
- Advanced therapies such as stem cell therapy and targeted drug therapy attack cancer at its source, improving patient care.
- Monoclonal antibodies and small molecule inhibitors target specific aspects of cancer cells, making treatments more effective.
- Ongoing research in gene editing and immunotherapy aims to provide even better options for fighting cancer in the future.
Overview of gene therapy for cancer treatment
Gene therapy is reshaping the fight against cancer by aiming to correct faulty genes responsible for disease development. This innovative approach utilizes various techniques, including the revolutionary CRISPR-based gene editing, to target and modify the genetic errors in cells that lead to cancer growth.
The U.S. Food and Drug Administration (FDA) has already approved multiple gene therapy products, highlighting its potential as a powerful tool in oncology treatment. By focusing on genetic mutations specific to an individual’s cancer, this method offers personalized treatment options, marking a significant advancement toward precision medicine.
The field of gene therapy promises a new frontier in battling cancer and signifies hope for treating other serious diseases like cystic fibrosis, heart disease, diabetes, hemophilia, and AIDS.
Its ability to directly address the root cause of these conditions—malfunctioning genes—presents an unprecedented opportunity in medical science. As researchers continue exploring its full potential through ongoing clinical trials and developments, gene therapy stands on the brink of transforming patient care and outcomes across a spectrum of diseases.
Gene therapy holds promise as a game-changer in medicine.
Importance of exploring new approaches and procedures
Exploring new approaches and procedures in cancer treatment opens doors to groundbreaking therapies that can save lives. Innovations like gene therapy offer hope against formidable diseases such as cancer, cystic fibrosis, and AIDS.
With the U.S. Food and Drug Administration approving multiple gene therapy products, there’s a growing recognition of its potential to change patient care fundamentally. These advanced treatments aim at specific genetic mutations in cancer cells, making personalized medicine more than a possibility—it becomes reality.
Precision medicine leverages unique genetic profiles to customize treatments for individual patients. Tools like CRISPR-based gene editing revolutionize how we approach genetic disorders by allowing precise modifications at the DNA level.
This shift towards highly targeted therapies exemplifies why constant research and development in fields like immunotherapy and genome editing are crucial. As these technologies mature, they could vastly improve outcomes for patients around the world, emphasizing the importance of pursuing these novel strategies relentlessly.
Purpose of the guide
This guide serves as a bridge between the complex world of gene therapy for cancer treatment and those who seek to understand it better. With breakthroughs in genetics offering up new hopes for targeting diseases at their root, it’s critical to grasp how these advancements might shape future treatments.
Gene therapy represents a revolutionary approach, tackling genetic mutations responsible for cancer by correcting them or altering genes to fight the disease. The U.S. Food and Drug Administration has given its nod to multiple gene therapy products, underscoring its potential impact on patient care outcomes.
The field is vast and rapidly evolving—precision medicine customizes treatment based on individual genes, while technologies like CRISPR have opened up incredible possibilities in genome editing.
By breaking down these concepts into digestible pieces, this guide aims to enlighten readers about the strides being made towards more personalized and effective cancer therapies. Knowledge of current FDA-approved therapies can empower patients with choices they may not have realized they had; understanding could be just what is needed for someone looking toward cutting-edge treatments.
Moving forward, we explore the specifics of gene therapy, laying out how it functions at a molecular level.
Understanding Gene Therapy
Gene therapy transforms the fight against cancer by directly fixing the genetic glitches that cause the disease. It offers a beacon of hope, opening new doors to personalized and effective treatments for patients battling cancer.
Definition of gene therapy
Gene therapy represents a cutting-edge medical approach focusing on modifying the genes inside a person’s cells to treat or prevent disease. This revolutionary method holds great potential, especially for conditions like cancer, cystic fibrosis, heart disease, diabetes, hemophilia, and AIDS.
By targeting the genetic flaws that contribute to disease, gene therapy offers hope for personalized treatments that go beyond the limitations of traditional medicines.
The U.S. Food and Drug Administration (FDA) has already given its nod to several gene therapy products aimed at cancer and rare diseases. With innovations like CRISPR-based gene editing and immune cell gene therapy leading the way, this field promises more precise interventions against diseases’ genetic causes.
Moreover, by harnessing tools such as genome editing and CAR T-cell therapy—methods used for reprogramming immune cells or correcting harmful mutations—gene therapy paves the way toward personalizing medicine based on individual genetic profiles.
Precision medicine is reshaping healthcare by offering care tailored to individual genetics.
Explaining genes and their role in cancer
Our bodies are made up of trillions of cells, each with its own set of genes. These genes act like tiny instruction manuals for how our cells should behave. Sometimes, a mistake in these instructions can cause a cell to grow and divide more than it should.
This uncontrolled growth can lead to cancer. It’s like having a typo in an important document that changes the whole meaning.
The role of genes in cancer doesn’t stop there. Cancer can be caused by genetic mutations passed down from our parents or by changes that happen during our lifetime due to external factors like smoking or too much sun exposure.
Gene therapy aims at fixing these typos in our cellular instruction manuals, offering hope against diseases including cancer—a leading cause of death worldwide. With gene therapy‘s promise shining brightly, researchers and healthcare providers are tirelessly working on making treatments more effective and accessible for all patients struggling against this formidable disease.
Types of gene therapy for cancer
Understanding how genes play a role in cancer sets the stage for exploring gene therapy. This innovative approach targets the genetic mutations behind cancer, aiming to treat or even prevent this disease.
- OncoVirus-Based Gene Therapy: Viruses are engineered to attack cancer cells without harming normal cells. The FDA has approved such treatments based on their ability to specifically target and kill cancerous tissues while sparing healthy ones.
- Gene Transfer: Healthy genes are introduced into a patient’s body to replace, inactivate, or knock out the malfunctioning genes responsible for cancer growth. This method directly targets the genetic abnormalities within cancer cells.
- CRISPR-Cas9 Gene Editing: Utilizes the CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) system for precision editing of DNA sequences in cancer cells. By correcting the genetic mutations that cause cancer, this approach offers a highly personalized treatment option.
- Immune Cell Gene Therapy: T-cells from a patient’s immune system are genetically modified to enhance their ability to identify and destroy cancer cells more effectively. CAR T-cell therapy is a notable example, where T-cells are engineered to seek out and attack specific cancer cell antigens.
- Oncolytic Virus Therapy: Employs viruses that selectively infect and kill cancer cells while stimulating an immune response against tumors. This dual action not only reduces tumor mass but also helps prevent recurrence by priming the immune system.
- Suicide Gene Therapy: Involves introducing genes into cancerous cells that make them susceptible to certain drugs that activate a cell death mechanism specifically within these modified cells, leaving normal cells unaffected.
- RNA Interference (RNAi) Therapy: Uses small pieces of RNA to silence specific genes associated with cancer development and progression. This technique can block the production of proteins essential for tumor growth.
- Antisense Oligonucleotides: Short DNA or RNA molecules designed to bind to mRNA molecules inside the cell and inhibit the production of proteins necessary for cancer cell survival.
Through targeting specific genetic mutations in each patient’s tumor, gene therapy provides individualized treatment options beyond conventional methods, marking a potentially transformative step forward in oncology treatment strategies.
Current Cancer Treatment Modalities
Doctors use many ways to fight cancer, including chemotherapy and radiation. Newer methods like stem cell therapy and targeted drugs also show promise.
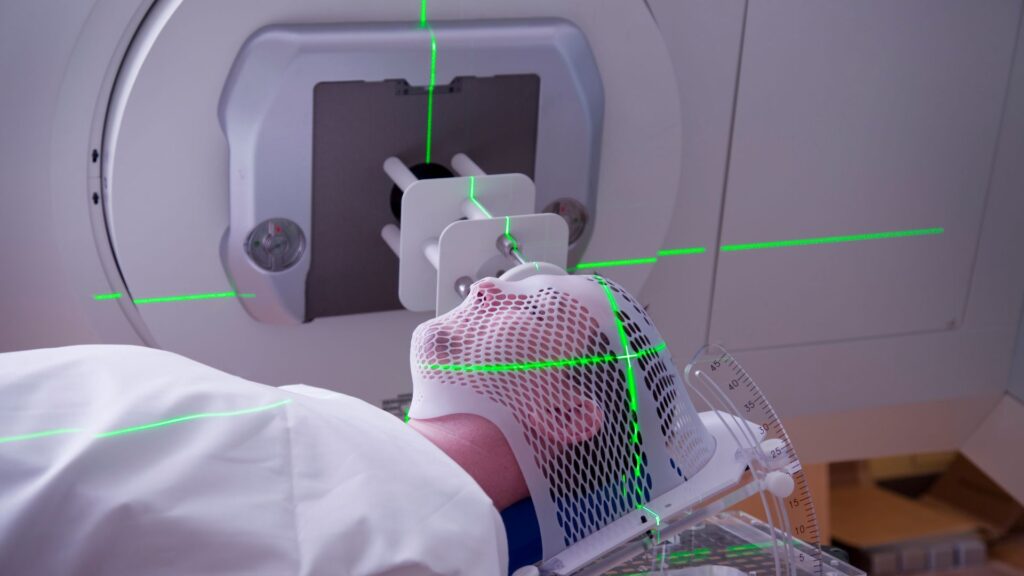
Conventional therapies such as chemotherapy and radiation
Chemotherapy and radiation stand as pillars in the fight against cancer, targeting rapidly dividing cells to reduce or eliminate tumors. These methods, while effective for many, can also harm healthy cells, leading to side effects like fatigue and hair loss.
The precision of these therapies has improved with advances in medical technology, allowing oncologists to minimize damage to surrounding tissues. Gene therapy represents a leap forward from these conventional treatments by aiming at the genetic blueprint of cancer itself.
As we explore further into gene therapy‘s potential, it becomes clear that this innovative approach seeks not just to destroy cancerous cells but to correct the underlying genetic mutations causing disease progression.
This marks a significant shift to personalized medicine where treatment is customized specifically to an individual’s genetic makeup—a strategy many experts believe is key in achieving long-term remission or even a cure for certain cancers.
Advanced and innovative therapies such as stem cell therapy and targeted drug therapy
Advanced and innovative therapies, like stem cell therapy and targeted drug therapy, are reshaping the fight against cancer. These treatments offer more precision in attacking cancer cells while sparing healthy tissues.
- Stem cell therapy relies on the power of pluripotent stem cells, which have the potential to turn into any type of cell in the body. This ability makes them invaluable for regenerating damaged tissues or organs affected by cancer.
- Adult stem cells, extracted from bone marrow or blood, are used to replenish the body’s supply of healthy cells destroyed by chemotherapy or radiation therapy.
- Cancer stem cells, a focus of current research, present a challenge as they can lead to relapse and metastasis. Targeting these cells is crucial for long-term cancer eradication.
- The FDA has endorsed several gene therapies that demonstrate the promising role of genetic manipulation in treating cancer effectively.
- Precision medicine takes center stage with therapies designed based on individual genetic profiles, ensuring treatments work best for each patient’s specific type of cancer.
- CRISPR-based gene editing techniques are at the forefront of customizing cell therapies. By cutting out cancer-causing genes from DNA sequences, scientists aim to stop cancer right at its source.
- Immunotherapy utilizes immune cell gene therapy to teach the body’s own immune system to fight off cancerous cells more efficiently.
- Targeted drug therapies act on specific molecular targets associated with cancer. Monoclonal antibodies and small molecule inhibitors disrupt the growth signals of tumor cells without affecting normal, healthy cells around them.
- CAR T-cell therapy represents a specific form of immune cell gene therapy where patient’s T-cells are engineered to better recognize and attack cancer cells after being reintroduced into their bloodstream.
- Ongoing clinical trials continue to explore natural antioxidants for their potential anti-cancer benefits alongside these advanced treatments, combining traditional wisdom with modern science for comprehensive care options.
Each advancement delivers hope—offering patients not just more years but better quality life during those years.
Stem Cell Therapy
Stem cell therapy stands as a frontier in cancer treatment, harnessing the body’s own cells to fight tumors. This innovative approach taps into the power of various stem cells to repair, regenerate, and even target cancerous growths directly.
Explanation of pluripotent, adult, and cancer stem cells
Pluripotent stem cells have the power to turn into any cell type in the body. They come from embryos or are made in labs using methods like CRISPR-based genome editing, a technique that has revolutionized cancer research and therapy.
These cells offer a broad platform for understanding how diseases start and for testing new drugs. On the other hand, adult stem (or somatic) cells exist throughout the body after development.
They specialize by replacing cells as they wear out or get damaged. Since they’re more limited than pluripotent stem cells, they mainly help repair and maintain tissues where they reside.
Cancer stem cells are tricky; they act like seeds for tumors, causing them to grow and spread through the body. This makes cancer hard to kill completely because these cells often resist treatment, hiding away only to grow back even after therapies like chemotherapy or radiation thought to be successful.
The FDA’s approval of gene therapy products targeting these resilient cancer mechanisms shows promise in offering new ways to tackle this challenge directly at the genetic level—ushering in personalized treatment options that could potentially transform patient care outcomes in oncology.
The potential of gene therapy lies in its ability to target specific genetic mutations within cancer cells.
Potential of stem cell therapy in cancer treatment
Stem cell therapy shows great promise for revolutionizing cancer treatment. This innovative approach can significantly impact patient care and outcomes by targeting the disease at its root.
Stem cells have the unique ability to develop into many different cell types in the body, making them powerful tools for regenerating damaged tissues or organs. For cancer patients, this means potentially replacing cells destroyed by chemotherapy or radiation with healthy ones, improving recovery times and reducing harmful side effects.
The U.S. Food and Drug Administration (FDA) has already approved multiple gene therapy products focusing on rare diseases and some cancers. With precision medicine paving the way, healthcare providers can offer more personalized care based on an individual’s genetic makeup, enhancing treatment efficacy.
The CRISPR system further highlights the potential of stem cell therapy in precisely editing genes within stem cells to fight cancer more effectively than ever before. As research in this area continues to grow, so does hope for developing more advanced treatments that could one day turn the tide against cancer altogether.
Moving onto targeted drug therapy,…
Targeted Drug Therapy
Targeted drug therapy attacks cancer cells directly without harming healthy ones. This method uses medicines to block the growth of cancer cells by targeting specific genes or proteins.
Types of targeted agents
Targeted drug therapy has transformed cancer treatment by directing medicines to attack cancer cells without harming surrounding healthy tissue. These agents focus on specific molecules and pathways involved in the growth and spread of cancer cells.
- Monoclonal Antibodies (mAbs): These are immune system proteins created in the lab to bind to specific targets found on cancer cells. For example, Trastuzumab targets the HER2 protein overexpressed in some breast cancers, helping to stop or slow cell growth.
- Small Molecule Inhibitors: This category includes drugs that can enter cells easily due to their small size and block certain enzymes and signals that tumors need to grow. Imatinib, used for treating chronic myeloid leukemia (CML), is one such drug targeting the BCR-ABL protein caused by a genetic mutation.
- Signal Transduction Inhibitors: These inhibitors block the activities of molecules that send signals from a cell’s surface to its interior, telling the cell to grow and divide. By blocking these signals, cancer cell growth is halted or slowed down. Sorafenib, which inhibits multiple signaling pathways in renal cell carcinoma, serves as an example.
- Angiogenesis Inhibitors: Cancer tumors need blood vessels to supply nutrients and oxygen for their growth. Angiogenesis inhibitors like Bevacizumab work by blocking the blood vessel formation process in tumors.
- Apoptosis Inducers: These drugs cause cancer cells to undergo apoptosis—a type of programmed cell death important for stopping cancer from growing. Bortezomib promotes apoptosis in multiple myeloma cells by disrupting various cellular processes.
- Immunomodulating Drugs: Leveraging the body’s immune system, these treatments enhance or suppress the immune response against cancer cells. Ipilimumab boosts the body’s immune response against melanoma cells by targeting CTLA-4, a protein on T-cells that normally helps keep the body’s immune reactions in check.
- Specific Genome Editing Tools: Techniques such as CRISPR-based gene editing target and modify genetic material directly within cancer cells or immune system cells designed to fight cancer more effectively.
- Hormone Therapies: Applied primarily in cancers sensitive to hormones like breast or prostate cancer, these therapies block the body’s ability to produce certain hormones or interfere with hormone action on tumor cells.
- Protein Degradation Inducers: This emerging class of targeted agents promotes degradation of abnormal proteins associated with tumor development or progression.
- Radioimmunotherapy Agents: Combining radiation therapy with immunotherapy, these agents deliver radioactive substances directly into cancer cells through antibodies linked with radioactive materials; this method allows focused radiation delivery at cellular levels.
Each type represents groundbreaking research and FDA approvals that have led to innovative treatments for various types of cancers, offering hope through personalized medicine based on genetic profiles of both disease and patient.
Role of monoclonal antibodies and small molecule inhibitors in cancer treatment
Monoclonal antibodies and small molecule inhibitors have revolutionized cancer treatment. They target cancer cells with precision, sparing healthy ones. This approach aligns with the FDA’s approval of multiple gene therapy products for cancer, highlighting their importance in medical advancements.
Monoclonal antibodies attach to specific targets on cancer cells, flagging them for destruction by the body’s immune system—a strategy that exemplifies immunotherapy‘s potential to kill cancer cells.
Small molecule inhibitors disrupt the signals that promote cancer cell growth and survival. They fit into the precise areas within or on the surface of cancer cells, like a key fits into a lock, blocking the pathways that allow cancers to thrive and multiply.
This method reflects how targeted drug therapy uses biological molecules identified through genetic medicine and genomic medicine research to halt disease progression. A notable mention is CRISPR-based gene editing—endorsed as a revolutionary tool by oncology treatment specialists—which can potentially be used alongside these inhibitors for more effective outcomes.
Moving forward, let’s explore how thermal ablation adds another layer to today’s multifaceted approach to combatting cancer.
Ablation Cancer Therapy
Ablation therapy attacks cancer in a direct way, focusing on killing or shrinking tumors. Doctors use tools like extreme cold or heat to target the bad cells without major surgery.
Overview of thermal ablation, cryoablation, and RFA therapy
Thermal ablation uses heat to destroy cancer cells. Often, doctors use it to treat tumors in the liver or kidneys. This method directs heat directly at the tumor, aiming to kill cancer cells without harming healthy tissue around them.
Cryoablation works differently—it freezes the cancer cells instead of heating them. A special tool cools down to very low temperatures, then is applied to target and kill tumor cells by freezing.
Radiofrequency ablation (RFA) therapy is another technique where high-frequency radio waves produce heat used to destroy abnormal cells. It’s particularly effective for patients who cannot undergo traditional surgery due to other health issues or when tumors are in hard-to-reach places.
The FDA has approved several methods, including RFA, as part of advancing treatments aimed at offering personalized options for cancer patients. These procedures highlight how precision medicine can tailor treatment based on individual patient needs and specificities of their disease, drawing upon key developments within gene therapy and immunotherapy fields for enhanced outcomes.
Effectiveness and limitations of ablation therapy
Building on the exploration of thermal ablation, cryoablation, and RFA therapy, we see how these treatments aim to control cancer. Ablation therapy can be quite effective in treating certain types of tumors.
It destroys them without needing open surgery. This makes recovery faster and reduces risks for patients. Most often used in cases like liver cancer, this method has shown significant benefits.
There are limitations, though. Ablation therapy may not work for all cancers or larger tumors. Sometimes, it cannot reach every cancer cell, which might lead to the disease coming back later.
Techniques like RFA require precision; missing even a small area can affect outcomes greatly.
Ablation therapies offer hope but remind us that one size does not fit all in cancer treatment.
Gene Therapy for Cancer Treatment
Gene therapy transforms the battle against cancer by targeting its genetic roots. It uses advanced techniques to repair or replace faulty genes, offering hope for more effective treatments.
Steps involved in gene therapy
Gene therapy represents a groundbreaking approach in the fight against cancer, offering new hopes and avenues for treatments that were once thought impossible. This innovative technique focuses on correcting or modifying genetic mutations to effectively treat or potentially cure cancer.
- Identification of Target Genes: Scientists first pinpoint the specific genes related to cancer growth or progression using advanced genomic technologies.
- Designing the Therapeutic Gene: Next, researchers design a therapeutic gene that can either repair, replace, deactivate, or introduce a new gene to help combat the cancer cells.
- Vector Selection: To deliver the therapeutic gene into the patient’s cells, a vector—usually a virus that has been genetically altered to be safe—is chosen because of its efficiency at entering cells.
- Lab Testing: Before any human trials can begin, extensive laboratory testing takes place to ensure safety and efficacy. This involves testing on cell cultures and animal models.
- Manufacturing the Therapy: Once proven in lab tests, the gene therapy is produced in larger quantities following strict FDA guidelines to ensure its quality and safety for human use.
- Regulatory Approval for Clinical Trials: Researchers must obtain approval from regulatory bodies like the FDA by presenting their lab results, proposed methods for delivering the therapy, and detailed plans for clinical trials.
- Conducting Clinical Trials: The therapy then undergoes rigorous clinical trials in three phases to test its safety, effectiveness, how well it works across different patient populations, and side effects.
- Data Analysis and FDA Review: After clinical trials are completed, scientists analyze all collected data. If results are promising, they submit everything to the FDA for review.
- Final Approval and Monitoring: Should the FDA find the gene therapy effective and safe; it grants approval making it available for public use while continuing to monitor its long-term effects and effectiveness.
Each step reflects an intricate blend of science, regulation, and patient care designed not just to extend lives but also improve their quality by tackling cancer at its genetic roots with precision medicine strategies.
Specific examples of gene therapy for cancer
Moving from the steps involved in gene therapy, we now explore concrete examples where this innovative treatment is making strides against cancer. The U.S. Food and Drug Administration (FDA) has approved several products that showcase the power of gene therapy in oncology treatment.
For instance, CAR T-cell therapy stands out as a groundbreaking approach. By modifying patients’ immune cells to attack cancer cells more effectively, this technique has transformed the outlook for certain blood cancers.
Another compelling example involves CRISPR-based gene editing technologies which have been pivotal in targeting specific genetic mutations within cancer cells. This precision medicine approach tailors treatments to individual patient’s genetic profiles, opening up pathways for more personalized and effective care options.
Through these examples—CAR T-cell therapy and CRISPR-edited technologies—the potential of gene therapy in revolutionizing cancer treatment becomes vividly clear, offering hope for better outcomes.
Natural Antioxidants and Clinical Trials
Exploring the role of natural antioxidants in fighting cancer has led to several clinical trials. These studies aim to uncover how these substances can best be used alongside traditional treatments.
Importance of natural antioxidants in cancer treatment
Natural antioxidants play a vital role in cancer treatment. They fight against cancer by protecting cells from damage caused by free radicals. These powerful substances can slow down the growth of cancer cells and make them more responsive to therapies like chemotherapy and radiation.
Antioxidants such as vitamins C and E, selenium, and carotenoids are proven to bolster the immune system’s ability to combat cancer.
Clinical trials have shown promising results with natural antioxidants in reducing side effects of traditional cancer treatments. Patients undergoing treatments often face less toxicity when antioxidants are part of their regimen.
This approach helps improve the quality of life for those fighting cancer and also opens up new avenues for making conventional treatments more effective and less harmful.
Current clinical trials and future possibilities
Current clinical trials are pushing the boundaries of what’s possible in cancer treatment. Scientists use innovative tools like CRISPR-based gene editing to target genetic mutations specific to cancer cells.
This approach offers personalized treatment, which could revolutionize patient care. The U.S. Food and Drug Administration has already approved several gene therapy products for cancer, showing significant promise for this technology.
The field is rapidly evolving with precision medicine at the forefront, enabling healthcare providers to tailor treatments based on an individual’s genetic makeup. With ongoing research into the immune system’s role in combating cancer, immunotherapy emerges as a key player.
Trials continue to explore how modifying immune cells through gene therapy can more effectively find and destroy cancer cells—marking a future where cancer treatment could be highly customized and more effective than ever before.
Conclusion
Explore more about the groundbreaking potential of gene therapy in cancer care. Stay informed, and keep learning about this innovative approach that continues to shape the future of oncology treatment.
Recap of key points in the guide
Gene therapy is making waves as a potential lifesaver for patients battling cancer and other serious diseases like cystic fibrosis, heart disease, diabetes, hemophilia, and AIDS. With the U.S. Food and Drug Administration’s approval of several gene therapy products for both cancer and rare disease treatments, the future looks bright.
Innovations such as CRISPR-based genome editing are revolutionizing our approach to medicine by targeting specific genetic mutations in cancer cells. This precision medicine allows healthcare providers to create treatment plans that are unique to each patient’s genetic makeup.
Immunotherapy stands out as it empowers the immune system to locate and destroy cancer cells effectively. The ongoing development within this field suggests a promising horizon where gene therapy could change how we treat cancer and a broad spectrum of illnesses.
Gene therapy aims at correcting or controlling defective genes responsible for disease progression, offering hope for personalized treatment options that directly address genetic anomalies in individuals.
As research advances rapidly in this field, it holds significant potential to improve patient care outcomes drastically.
Encouraging further research and development in gene therapy for cancer treatment
Moving forward, the journey from understanding gene therapy as a revolutionary cancer treatment to its implementation is pivotal. Gene therapy offers hope against diseases like cancer, heart disease, and diabetes.
Its potential in modifying or repairing defective genes to treat or prevent diseases marks a significant advancement in medicine. The U.S. Food and Drug Administration has already recognized this by approving multiple gene therapy products for cancer treatment.
The promise of precision medicine lies in offering personalized care based on an individual’s genetic makeup. With CRISPR technology revolutionizing genome editing, specific genetic mutations in cancer cells can be targeted more effectively than ever before.
This hints at individualized treatment options that could drastically improve patient outcomes. Encouraging more research into gene therapy supports the development of innovative treatments and lays down a pathway for curing various genetic disorders that impact millions worldwide.
FAQs
1. What is gene therapy for cancer treatment?
Gene therapy for cancer treatment, well, it’s a way doctors try to fix or replace genes in your cells to fight or prevent cancer.
2. Can anyone get gene therapy for cancer?
Not everyone can get it right now — doctors decide based on the type of cancer and how advanced it is.
3. How does gene therapy work against cancer?
It works by either fixing damaged genes that cause disease, adding new genes to help fight the cancer, or making those bad cells easier for your immune system to find and destroy.
4. Are there side effects with gene therapy?
Yes, there can be side effects like fever or tiredness, but these depend on the type of gene therapy you’re getting.
5. How long does it take to see if the gene therapy is working?
The time varies; some people might see results in a few weeks, while others may take longer to know if it’s really kicking in against the cancer.
General Facts
- Gene therapy holds promise as a treatment for a wide range of diseases, including cancer, cystic fibrosis, heart disease, diabetes, hemophilia, and AIDS.
- The field of gene therapy promises innovative treatments that are likely to become important in preventing deaths from cancer.
- Immunotherapy is a cancer treatment that uses the immune system to find and kill cancer cells.
- Gene therapy aims to control the altered genes or genetic mutations of cancer to prevent its growth.
- The U.S. Food and Drug Administration has approved multiple gene therapy products for cancer and rare disease indications.
- Precision medicine is a way for healthcare providers to offer specific care for patients based on their particular genes.
- The CRISPR system is a revolutionary genome editing tool with the potential to revolutionize the field of cancer research and therapy.
- Gene therapy has shown promise as a treatment for cancer and has the potential to be a game-changer in the field of medicine.
- Gene therapy can be used to target specific genetic mutations in cancer cells, providing personalized treatment options for patients.
- The development of gene therapy for cancer treatment is an exciting and rapidly evolving field with the potential to significantly impact patient care and outcomes.
Source URLs
- Understanding Gene Therapy: Mayo Clinic Overview
- Insights into Gene Therapy Research: PubMed Article
- Exploring Immune Cell Gene Therapy: WebMD Article
- Advancements in Cancer Treatment: Gene Therapy: ACGT Foundation
- Understanding Gene Therapy’s Potential: FDA Consumer Update
- Precision Medicine in Cancer Treatment: American Cancer Society
- Gene Therapy’s Role in Cancer Research: Molecular Cancer Journal











