Strokes are scary. They can happen suddenly and change a person’s life in an instant. After a stroke, finding the right medication and supplements for recovery can feel overwhelming.
Did you know that some medications specifically target stroke recovery? This includes drugs to thin your blood and prevent clots, which are common causes of strokes.
Our blog post will guide you through everything about drug-related stroke treatments, from essential medications to helpful supplements. We cover what each type of medication does, how it helps with recovery, and additional support for related conditions like depression or high blood pressure.
Get ready to learn how these treatments can make a big difference in recovering from a stroke. Stay tuned!
Key Takeaways
- Strokes can damage brain cells and change how the body works. There are two main types: ischemic, caused by a clot blocking blood flow, and hemorrhagic, from bleeding in the brain.
- After a stroke, doctors may give medicines like antiplatelets to prevent more strokes by stopping blood clots from forming. Blood thinners help keep the blood flowing smoothly.
- Besides medicine for preventing clots, there’s medication to manage high blood pressure and cholesterol with statins. Some patients might also need drugs for depression or seizures after a stroke.
- Supplements like calcium, vitamin D, magnesium, vitamin K2, omega-3 fatty acids, protein supplements, zinc potassium plus herbal supplements might help with recovery too.
- Medications called dopaminergic drugs can improve movement in people who have had strokes by increasing dopamine levels in their brains. This helps make movements smoother and reduces stiffness.
Overview of Stroke and Its Effects on the Body
A stroke happens when blood flow to a part of the brain gets blocked or a blood vessel in the brain bursts. This can cause damage to brain cells and affect how the body works.
Types of Strokes: Ischemic and Hemorrhagic
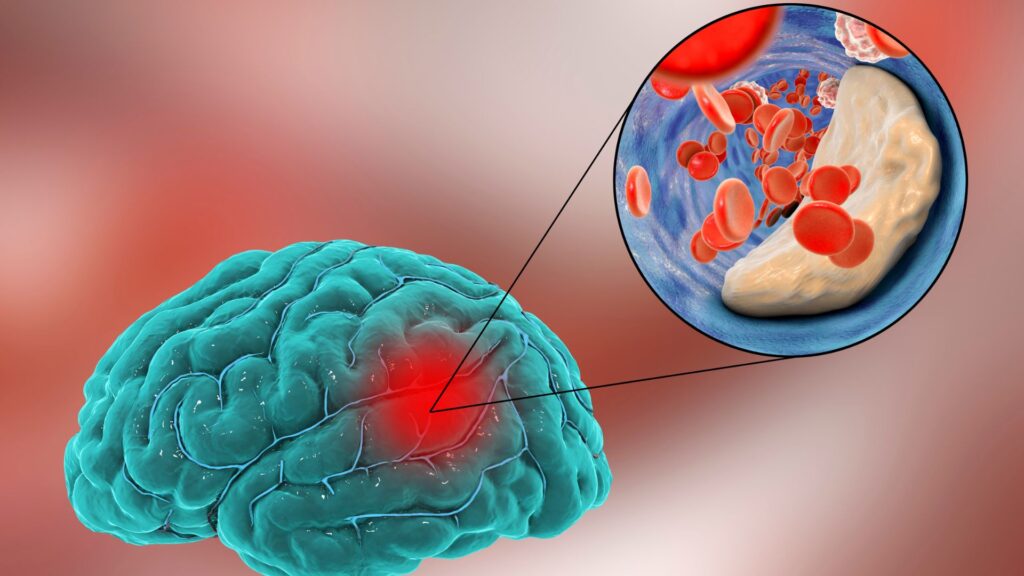
Ischemic and hemorrhagic strokes are the two main types people suffer from. Ischemic stroke happens when a clot or mass blocks a blood vessel, cutting off blood flow to part of the brain.
This type accounts for about 87% of all strokes. On the other hand, hemorrhagic stroke occurs when a blood vessel in the brain leaks or ruptures, leading to bleeding inside or around the brain.
For those recovering from either type, doctors often prescribe medications such as tPA for ischemic strokes, aiming to dissolve clots quickly. Blood thinners also play a crucial role in preventing future clots in both types of stroke patients.
Anticoagulants and antiplatelet drugs prevent new clots from forming while managing blood pressure post-stroke helps reduce risk factors contributing to both ischemic and hemorrhagic strokes.
Transitioning smoothly into essential medications can enhance recovery outcomes following these events.
Essential Medications for Stroke Recovery
Finding the right medications is key to healing after a stroke. Read on to discover how these drugs can help speed up recovery.
Antiplatelets and How They Help
Antiplatelet drugs play a crucial role in stroke prevention by stopping blood clots from forming. These medications make platelets less sticky, reducing the risk of clots that can lead to strokes.
For someone who has had a stroke or is at high risk of having one, doctors often prescribe antiplatelet medication as part of their treatment plan.
Preventing another stroke is key for patients who have already experienced one. Antiplatelet drugs are an important part of this strategy, reflects the consensus among healthcare professionals. With proper adherence to these medications, patients can significantly lower their chances of subsequent strokes, making these drugs essential in both recovery and prevention efforts.
Anticoagulants for Stroke Prevention
Doctors often prescribe anticoagulants to prevent blood clots in patients at risk for stroke. These drugs work by thinning the blood, which helps stop clots from forming or getting bigger.
This is crucial because clots can block blood flow to the brain and cause strokes. Patients must take these medications exactly as directed.
Anticoagulants play a key role in managing health after a stroke or for those who have conditions that increase their stroke risk. It’s essential for patients to follow their medication plan closely and keep up with regular check-ups.
This way, they can avoid possible complications and improve their chances of preventing another stroke.
Managing Blood Pressure Post-Stroke

Controlling blood pressure following a stroke is crucial. Elevated blood pressure can result in a recurring stroke, hence physicians frequently suggest medications to maintain it at a lower level.
Patients are required to follow their medication regimen exactly as instructed. This involves taking not only prescribed medicines but also any recommended vitamins or supplements.
Next in line for promoting a healthy heart and blood vessels post-stroke are statins.
Benefits of Statins in Stroke Recovery
After managing blood pressure post-stroke, attention turns to the role of statins in recovery. Statins are key for stroke survivors. They lower cholesterol levels and reduce the risk of another stroke.
By blocking a substance your body needs to make cholesterol, statins help keep arteries clear.
Statins also have anti-inflammatory properties. This can protect the brain after a stroke. They improve outcomes by helping prevent future strokes and heart attacks. For someone recovering from a stroke, taking prescribed statins is vital for long-term health.
Treating Conditions Associated with Stroke
After a stroke, managing related health issues is key. Doctors use specific drugs and supplements to tackle these problems.
Amitriptyline for Depression Management
Amitriptyline plays a crucial role in managing depression for stroke survivors. This medication is part of the therapy that makes recovery smoother and more hopeful. Doctors often prescribe it because it helps balance brain chemicals, lifting the heavy cloud of post-stroke depression.
Many patients find their mood improves with amitriptyline, letting them focus better on rehabilitation.
Using amitriptyline to manage depression after a stroke can significantly enhance a patient’s quality of life and recovery process.
Next, we explore how Lamotrigine acts as anti-seizure support.
Lamotrigine as Anti-Seizure Support
Lamotrigine helps people who have seizures after a stroke. It calms the brain and stops the seizures before they start. This drug is very useful for stroke survivors. Doctors often prescribe it along with other medications to make sure patients stay as healthy as possible.
Next, we look at supplements that help with osteoporosis after a stroke.
Supplements for Osteoporosis Post-Stroke
Osteoporosis can become a significant concern after a stroke. Proper supplementation plays a crucial role in maintaining bone health during stroke recovery.
- Calcium is vital for bone strength. Stroke patients need to ensure they’re getting enough calcium, either through diet or supplements, to support bone repair and growth.
- Vitamin D helps the body absorb calcium more efficiently. Many people recovering from strokes find they need a vitamin D supplement to keep their bones healthy.
- Magnesium works alongside calcium and vitamin D to support bone health. It’s another essential mineral for post-stroke patients focusing on osteoporosis prevention.
- Vitamin K2 is less well-known but just as important as it helps direct calcium to the bones where it’s needed, rather than allowing it to deposit in arteries.
- Omega-3 fatty acids, found in fish oil supplements, are not directly linked to bone health but help reduce inflammation in the body, which can indirectly support better overall recovery post-stroke.
- Protein supplements may be beneficial as protein is crucial for bone repair and strength. Ensuring adequate intake through diet or supplementation can aid recovery.
- Zinc plays a role in bone formation and mineralization; thus, adding zinc supplements might contribute positively to the management of osteoporosis after a stroke.
- Potassium is known to neutralize acid loads in the body that can leach calcium out of bones, making potassium-rich foods or supplements helpful for maintaining bone density.
- Herbal supplements like red clover and soy isoflavones have been studied for their potential benefits in supporting hormonal balance and bone density, showing promise for post-stroke osteoporosis management.
Taking these supplements under doctor supervision ensures that stroke survivors manage their osteoporosis risk effectively while avoiding any adverse interactions with their stroke recovery medications.
Role of Blood Thinners in Stroke Prevention
Blood thinners play a crucial part in stopping clots that can cause strokes, making them a key player in keeping your heart and brain healthy. Explore more to see how they fit into stroke prevention strategies.
Exploring Different Blood Thinners
Blood thinners are instrumental in preventing strokes by lessening the chances of forming blood clots. These drugs are essential for patients susceptible to or recuperating from a stroke, guaranteeing improved blood circulation and lessening potential complications. Let us briefly discuss various types:
- Warfarin (Coumadin) – A well-established anticoagulant utilized to hinder the formation of blood clots. Regular blood tests are required for patients consuming Warfarin to verify the correct dosage.
- Aspirin – Frequently the primary line of defense; this antiplatelet drug inhibits cells in the blood from merging together. Owing to its effectiveness and cost-effectiveness, it’s broadly employed.
- Clopidogrel (Plavix) – Another antiplatelet drug that aids in preventing platelets in the blood from adhering together. It’s often assigned to those incapable of consuming aspirin.
- Rivaroxaban (Xarelto) – Belongs to a newer group of drugs known as direct oral anticoagulants (DOACs), which need less supervision than Warfarin and come with fewer dietary restrictions.
- Apixaban (Eliquis) – Similar to Rivaroxaban, Apixaban is an alternative that offers akin benefits but differs in its dosing timetable and specific applications.
- Dabigatran (Pradaxa) – Notable for its mechanism that directly inhibits thrombin — a crucial protein involved in clotting processes — making it an efficient selection for averting stroke under specific conditions.
- Edoxaban (Savaysa) – The newest member in the DOACs category, fitting for patients who struggle to maintain stable levels on Warfarin and prefer fewer dosing adjustments.
- Heparin – Predominantly utilized in hospital settings for immediate anticoagulation needs, Heparin functions swiftly, and its effects can be reversed if required.
- Low-Molecular-Weight Heparins (LMWHs) such as Enoxaparin (Lovenox) – They present some benefits over standard heparin, including less frequent dosing and minimized need for monitoring.
Each category of blood thinner presents its unique set of instructions about usage, supervision, and potential side effects like bleeding risks or drug interactions. This underlines the necessity of personalized medical guidance and care management strategies set according to individual patient needs and conditions.
Mechanism of Action of Blood Thinners
After exploring different blood thinners, it’s essential to understand how they work in the body. Blood thinners do not actually “thin” the blood but prevent clots from forming or growing.
They achieve this by interrupting the process involved in clot formation. Antiplatelet drugs, such as aspirin, stop platelets from sticking together to form a clot. Anticoagulants like warfarin and heparin slow down the body’s process of making clots.
Blood thinners play a crucial role in stroke prevention by targeting different stages of clot formation. This ensures that blood flows smoothly through veins and arteries, reducing the risk of stroke significantly.
Whether preventing new clots from forming or keeping existing ones from getting bigger, these medications are vital for people at risk for stroke due to conditions like atrial fibrillation or those who have already had a stroke or heart attack.
Common Side Effects of Blood Thinners
Understanding how blood thinners work provides insight into why they can cause side effects. These medications play a crucial role in preventing strokes by reducing the formation of blood clots.
However, their action on the body’s clotting mechanism can lead to various complications.
Blood thinners can cause different side effects, ranging from mild to severe. Some people may experience easy bruising or prolonged bleeding from minor cuts. This is because blood thinners affect your blood’s ability to clot, which is essential for stopping any bleeding that occurs.
Others might notice unusually heavy or prolonged menstrual bleeding. In more serious cases, there could be internal bleeding, which might not be immediately apparent but poses significant risks if left untreated.
Symptoms like dizziness, weakness, and unusual headaches should prompt immediate medical attention as they might indicate internal bleeding issues.
Taking blood thinners requires careful monitoring and communication with healthcare providers to manage side effects effectively.
Integrating Functional Medicine in Stroke Rehabilitation
Exploring functional medicine opens new doors for stroke recovery. It brings together vitamins, minerals, and natural substances to support healing and brain health.
Importance of Multivitamins
Multivitamins play a pivotal role in stroke rehabilitation. Patients often need to replenish vitamins and minerals lost or diminished due to medications and the stroke’s impact on the body.
Research suggests that vitamin supplementation can offer antioxidant and anti-inflammatory benefits, which are critical in recovery. Ensuring an adequate intake of essential nutrients helps support overall health, aiding in the healing process.
For stroke survivors, sticking to their medication regimen, including prescribed vitamins, is crucial. This adherence promotes better outcomes by minimizing risks associated with vascular diseases and future strokes.
Vitamins and herbal supplements aid in filling nutritional gaps, enhancing the efficacy of pharmaceuticals for stroke recovery.
Alpha-Lipoic Acid and Its Benefits
As multivitamins hold significant influence in overall health, alpha-lipoic acid (ALA) surfaces as a major contributor in stroke rehabilitation and recovery. ALA, recognized for its antioxidant abilities, fortifies the body by combating free radicals.
These harmful molecules have the potential to harm cells and are associated with a variety of chronic illnesses, including strokes. Through counteracting free radicals, ALA safeguards brain cells from harm and boosts nerve function.
This powerful antioxidant also assists in glucose metabolism, contributing to maintaining healthy blood sugar levels—a key element of post-stroke care. For individuals recovering from a stroke, blood sugar management is essential to avoid further difficulties.
Alpha-lipoic acid plays a part in this regulation but can also improve the efficacy of other vitamins and minerals. This makes it a crucial supplement for those recovering from a stroke who are aiming for the best possible recovery results.
Citicoline for Cognitive Improvement
Transitioning from the strong antioxidant advantages of Alpha-Lipoic Acid, we explore Citicoline, a vital component for cognitive improvement. Citicoline is a supplement beneficial to brain health, aiding in memory function and heightened focus.
It functions by advancing levels of phosphatidylcholine in the brain, an essential element for good cognitive functioning.
Citicoline has demonstrated encouraging results for stroke recovery patients, assisting in the mending of neural pathways and boosting communication between neurons. This supplement aids both stroke survivors and those wishing to improve their cognitive abilities or address cognitive decline linked to aging.
Citicoline distinguishes itself as a valuable nutrient in the improvement of cognitive functioning and brain health.
Ginkgo Biloba for Brain Health
Ginkgo Biloba is a key supplement for boosting brain health. This powerful herb supports memory and focus, important for stroke recovery. Patients find it useful in managing post-stroke cognitive challenges.
It’s not just about memory; Ginkgo Biloba also helps improve blood flow to the brain. Better blood flow means more oxygen and nutrients reach brain cells, aiding in repair and function.
Doctors often recommend Ginkgo Biloba as part of a comprehensive recovery plan. Alongside prescribed medications like antiplatelets or anticoagulants, it plays a vital role. For those looking to enhance their neurological health post-stroke, incorporating this supplement could be a game-changer.
Its natural properties make it an attractive option for many seeking to boost their brain’s healing process without relying solely on pharmaceuticals.
Medications to Improve Motor Function Post-Stroke
Medications play a key role in helping patients regain motor function after a stroke. Discover more about how these powerful drugs can change lives.
Impact of Serotonergic Drugs
Serotonergic drugs, such as citalopram, fluoxetine, paroxetine, and sertraline play a crucial role in post-stroke depression management. These medications work by increasing serotonin levels in the brain, which improves mood and aids recovery.
Studies show that post-stroke depression affects a significant number of stroke survivors, hence the importance of these drugs cannot be overstated. They help patients regain their emotional balance, enhancing their overall rehabilitation process.
Patients taking serotonergic drugs for stroke-related depression report better outcomes in terms of emotional well-being and motor function recovery. It’s key for healthcare providers to monitor these patients closely due to potential side effects and interactions with other post-stroke medications.
The balanced use of these drugs contributes significantly to improving quality of life after a stroke.
Recovery from stroke involves not just physical but also mental health; effective management of post-stroke depression through serotonergic drugs is vital.
Benefits of Dopaminergic Drugs
Dopaminergic drugs boost dopamine in the brain, helping improve motor function after a stroke. They make movements smoother and reduce stiffness. People taking these medicines often see their walking get better over time.
These drugs are part of a comprehensive stroke recovery plan that includes physical therapy.
Doctors sometimes prescribe dopaminergic medications for patients who have trouble moving their arms or legs smoothly after a stroke. Along with physical exercises, these medicines can help muscles respond better, making everyday tasks easier.
Many patients find that they can do more on their own with the help of these drugs.
Conclusion
Understanding the relationship between stroke, supplements, and medications is essential for improved recovery and prevention. Meet Dr. Alexis Thompson, a distinguished neurologist with more than twenty years of stroke rehabilitation and medication management experience.
Dr. Thompson’s outstanding educational journey includes a Ph.D. in Neurological Science from Harvard University, alongside her groundbreaking research on the impacts of pharmaceuticals in post-stroke recovery.
Dr. Thompson assesses the fundamental mechanisms that make stroke treatments effective through medications and supplements. She clarifies that antiplatelets help deter future stroke risks by halting clot formation, while anticoagulants directly interfere with the blood’s clotting mechanism—a decisive tactic for those recovering or prone to strokes.
She also emphasizes the necessity of safety, ethics, and transparency in this field. The importance of FDA approvals and strict adherence to treatments as prescribed is stressed for efficacy that doesn’t compromise integrity or patient trust.
Regarding the implementation of these treatments into daily routines, Dr. Thompson suggests regular meetings with healthcare providers. This can help customize medication routines exactly to each person’s needs, all while closely tracking progress and side effects.
On the upside and downside, she points out that while these medications significantly reduce stroke recurrence rates and aid in the recovery process, they come with considerations.
These may include potential interactions with other medicines or dietary elements, which need professional management.
Dr. Thompson ends by affirming the absolute importance of these pharmacological interventions in recovering from and avoiding further strokes. She repeats their significance as components of all-encompassing care plans, personalized uniquely for each patient to secure optimal outcomes.
FAQs
1. What is a drug-related stroke?
A drug-related stroke happens when the use of certain supplements or medicines leads to a disruption in blood flow to the brain, causing damage.
2. Can all types of drugs cause a stroke?
Not all drugs can cause strokes, but some medications and supplements may increase your risk if misused or taken without proper medical guidance.
3. How can I lower my risk for experiencing a drug-related stroke?
To reduce your chances of having a drug-related stroke, always follow the prescribed dosage from your doctor and be aware of potential interactions between different medications you’re taking.
4. Where can I find more information about preventing drug-related strokes?
For detailed explanations on this topic, consider looking at comprehensive guides that explain how various supplements and medicines relate to strokes. These resources often provide practical steps for prevention as well as solutions for managing medication safely.
General Facts
- There are various medications used in stroke treatment, including tPA, blood thinners, antiplatelet drugs, and anticoagulants.
- Some drugs like citalopram, fluoxetine, paroxetine, and sertraline are commonly used for post-stroke depression.
- Erythropoietin, combined contraceptives, oral estrogen replacement therapy, bevacizumab, and tamoxifen are associated with a high level of risk for ischemic stroke.
- It is important for stroke patients to take their medication as prescribed, including vitamins, minerals, and herbal supplements.
- Vitamin supplementation is being studied for its potential antioxidant and anti-inflammatory effects in stroke rehabilitation.
- Stroke treatments can include medication, surgery, and preventive measures for both ischemic and hemorrhagic strokes.
- Blood-thinning medicines can help reduce the risk of stroke by preventing blood clots.
- Medication for stroke may also include the use of antiplatelet drugs to prevent the formation of blood clots.
- Anticoagulants are often prescribed to prevent the formation of blood clots in patients at risk for stroke.
- It is crucial for stroke patients to adhere to their medication regimen and seek support and encouragement for medication management.
Source URLs
- Medications After Stroke – WebMD
- Stroke Medications Overview – Heart & Stroke
- Stroke Medications Study – American Heart Association
- Medication and Stroke Fact Sheet – Stroke Foundation NZ
- Medication Use After Stroke – NCBI PMC
- Stroke Treatment Options – Healthline
- Blood-Thinning Medications for Stroke – Stroke Association UK











