Understanding Alzheimer’s disease can feel overwhelming. Many people worry about how to manage the condition, both for themselves and their loved ones. The good news is that while there is no cure for Alzheimer’s, certain treatments can help control symptoms and improve quality of life.
One important fact to keep in mind: clinical studies have played a crucial role in developing medications that ease cognitive decline associated with this disease. In our guide, we’ll dive into various medical treatments approved by the U.S. Food and Drug Administration (FDA), as well as supplement options that might offer additional benefits.
From understanding early-stage interventions to exploring potential vitamins and dietary supplements like omega-3 fatty acids, we aim to equip you with knowledge to make informed decisions.
Let’s explore together—your journey starts here.
Key Takeaways
- Alzheimer’s disease affects the brain, making it hard for people to remember things and do daily tasks. Special tests like brain scans help doctors diagnose it.
- There are medicines that can slow down Alzheimer’s symptoms. Some of these include cholinesterase inhibitors and memantine, which help with memory loss and thinking problems.
- Alternative treatments like omega-3 fatty acids, caprylic acid from coconut oil, and supplements such as Coenzyme Q10 might also support brain health in people with Alzheimer’s.
- Creating a safe home environment is crucial for someone with Alzheimer’s. This includes adding brighter lights, removing tripping hazards, and installing handrails in important areas.
- Doctors recommend careful consideration before using some medications because they can cause harm or have side effects that outweigh their benefits.
Overview of Alzheimer’s Disease
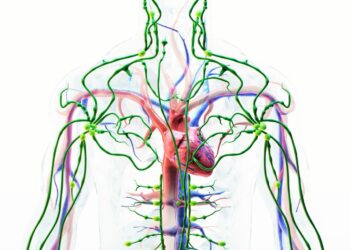
Alzheimer’s disease messes with the brain, making it hard for people to remember stuff and do everyday things. Doctors use special tests like brain scans to figure out if someone has it.
Definition and Nature
Alzheimer’s disease is a brain disorder that slowly destroys memory and thinking skills. People with this condition have trouble doing everyday things. Over time, they may not recognize family members or have conversations.
The disease involves the buildup of amyloid plaques and tau proteins in the brain. These substances harm the nerve cells, making it hard for them to talk to each other.
Scientists use MRIs and PET scans for diagnosis. They look at images of the brain to see if these harmful buildups are there. Finding Alzheimer’s early helps doctors manage symptoms better.
Understanding Alzheimer’s begins with recognizing it as more than just memory loss; it’s a decline in cognitive functions, severely impacting daily living.
Risk Factors
Some people are more likely to get Alzheimer’s disease because of certain risk factors. Age is the biggest one. Most people with this illness are over 65, but it can also happen in younger folks through early-onset Alzheimer’s.
Family history plays a role too; if your mom, dad, or sibling has it, you might have a higher chance of getting it as well. Genes like APOE-e4 can increase that risk even further.
Things like head injuries, sleep disturbances, and high blood pressure might also bump up your chances. Living a healthy lifestyle could help lower some risks – think regular physical activity and eating foods good for the brain.
Next up: Let’s talk about how doctors find out if someone has Alzheimer’s disease.
Common Symptoms
People with Alzheimer’s disease often forget things. They might forget names or why they walked into a room. This is called memory loss and it’s a big sign of the condition. They also have trouble doing simple tasks, like paying bills or following recipes.
These activities used to be easy for them.
Their mood changes too. One minute they’re happy, the next they’re sad or mad for no clear reason. It gets hard for them to follow conversations and find the right words when speaking or writing.
Some folks even see things that aren’t there, which can be scary. These symptoms make daily life tough not just for those with Alzheimer’s but also for their families who help take care of them.
Methods of Diagnosis
Doctors use several tests to find out if someone has Alzheimer’s disease. First, they talk to the person and their family about any memory problems or changes in behavior. This helps them understand what’s going on.
Next, doctors might ask the person to take a mini-mental state examination. This test checks how well their brain is working by asking simple questions and giving easy tasks. They also do physical exams and tests to rule out other causes for the symptoms.
To see inside the brain, doctors use imaging techniques like computerized tomography or positron emission tomography (PET). These scans help them spot any unusual patterns or areas of damage in the brain that are common with Alzheimer’s.
Sometimes, they check the cerebrospinal fluid—the liquid around your brain and spine—for signs of Alzheimer’s disease. Looking at this fluid can tell doctors if there are biomarkers—substances that suggest someone might have Alzheimer’s.
Doctors keep looking for better ways to diagnose Alzheimer’s early and accurately because catching it early means treatments can start sooner.
Understanding is the first step towards overcoming.
Medical Approaches to Treating Alzheimer’s Disease
Doctors use many ways to help people with Alzheimer’s disease feel better. They give them special medicines that can slow down the illness, handle mood swings, and improve memory for a while.
These methods include giving patients medicine pills and teaching caregivers how to deal with tough behaviors. Scientists are also working on new treatments that could do even more in the future.
Want to learn all about these options? Keep reading!
Treatment for Early to Mid-Stage Alzheimer’s
For those in the early to mid-stages of Alzheimer’s, doctors often recommend a group of drugs known as cholinesterase inhibitors. These include donepezil (Aricept), which can help manage memory loss, language breakdowns, and other cognitive issues.
They work by boosting levels of a chemical messenger involved in memory and judgment. While these medicines don’t cure Alzheimer’s, they can slow down its progression and make symptoms less severe.
Another medication option is memantine (Namenda), targeting the NMDA receptors in the brain. This approach helps control symptoms by regulating glutamate, an important neurotransmitter for learning and memory.
Memantine is usually prescribed when Alzheimer’s reaches moderate to severe stages but can also be used alongside cholinesterase inhibitors for earlier stages. Side effects like confusion or dizziness are possible but managing dosage properly often reduces these risks.
Advanced Alzheimer’s Medications
Doctors often prescribe strong medications for people with advanced Alzheimer’s. These drugs aim to help manage symptoms and improve quality of life. One group of these medicines includes acetylcholinesterase inhibitors, which work by boosting levels of a chemical messenger involved in memory and judgment.
Although there’s no cure, treatments like memantine—an N-methyl-D-aspartate receptor antagonist—can also help slow down the progression by targeting a different brain pathway.
Side effects like nausea or restlessness may occur, so it’s critical to follow dosage guidelines from healthcare providers carefully. For some people, antipsychotic drugs such as olanzapine, risperidone, or quetiapine might be necessary to control symptoms related to aggression or delusions.
Keeping close communication with doctors helps ensure that the benefits of these medications outweigh any risks, including potential issues like an increased risk of stroke or brain swelling in vulnerable patients.
Dosage Guidelines and Side Effects
After discussing advanced Alzheimer’s medications, let’s talk about how to use them right. The FDA approves drugs with specific dosages for safety and effectiveness. Each person may need a different amount based on their condition and other medicines they take.
Some drugs used for mild cognitive impairment or early stages might have clearer guidelines than others.
Side effects can vary too. For example, some common ones include nausea, insomnia, or even more serious issues like bleeding in the brain from certain prescription drugs. It’s key to report any new symptoms to a doctor quickly.
They can adjust the treatment or suggest ways to manage side effects better. Plus, staying informed about clinical trials could offer access to new treatments with potentially fewer side effects.
Behavior Management Techniques
Moving from understanding the dosage guidelines and side effects, we see the essential role of behavior management techniques. These strategies help deal with challenges like anger and confusion often faced by those with Alzheimer’s disease.
Caregivers use simple tasks to keep daily routines smooth. They also create a calm environment to reduce stress for both themselves and their loved ones.
Change is hard at first, messy in the middle, and gorgeous at the end.
Reducing noise can help prevent agitation. Using gentle reminders rather than arguments makes communication clearer. Activities such as walking or listening to music provide comfort and improve mood.
This approach not only supports individuals in maintaining their dignity but also offers caregivers effective ways to manage difficult moments without resorting to heavy medication or physical restraints.
Medications Requiring Caution
After exploring how to manage behavior in Alzheimer’s patients, it’s crucial to talk about medications that need careful use. Some drugs can cause more harm than good for those with Alzheimer’s disease.
For instance, certain “atypical antipsychotics” used to calm agitation can increase the risk of heart problems and even death in older adults. It’s wise for caregivers and doctors to weigh these risks carefully.
Doctors also caution against some over-the-counter remedies that promise brain health benefits. Products like “memory enhancers” might interact badly with FDA-approved Alzheimer’s drugs or lead to unexpected side effects.
Always check with a healthcare provider before starting any new supplement or medication, especially if you’re caring for someone with this condition. This ensures safety and avoids complications that could worsen symptoms or bring on new health issues.
Innovations in Treatment
Moving from the need for caution with certain medications, scientists and doctors are now focusing on cutting-edge treatments. They’re exploring how new drugs can offer hope to those fighting Alzheimer’s disease.
Some of these innovations include treatments that aim to target and reduce the buildup of amyloid plaques in the brain, a hallmark sign of this condition. These advancements are part of ongoing research efforts, aiming to slow down or even stop the progression of Alzheimer’s.
Clinical trials play a crucial role in discovering these new options. Phase 3 clinical trials are testing promising drugs that could change how we treat Alzheimer’s disease. One such drug under investigation aims to improve connections between nerve cells in the brain, potentially helping preserve memory longer.
These trials not only give us valuable data but also bring us closer to finding effective treatment solutions. With each step forward in research, there is growing optimism about developing therapies that can make a real difference for those living with Alzheimer’s disease.
Exploring Alternative Treatments
Looking into different treatments sheds light on new ways to help with Alzheimer’s. This includes everything from oils you can eat, to herbs, and even vitamins that might make a big difference.
Evaluating Non-Traditional Therapies
Looking into non-traditional therapies offers a new path for those battling Alzheimer’s disease. Many turn to herbal remedies, dietary supplements like omega-3 fatty acids, and activities that promote a healthy brain.
These alternatives draw attention for their potential to ease symptoms or even slow down the progression without the heavy side effects often seen with prescription drugs. The National Institute on Aging and various clinical trials put these methods under the microscope to verify their effectiveness.
Exploration is the essence of the human spirit. Just as this quote inspires us to venture beyond known boundaries, evaluating non-traditional therapies pushes us to discover new ways of supporting cognitive health in Alzheimer’s disease. From caprylic acid found in coconut oil to antioxidants like Coenzyme Q10, these options represent hope for many. The FDA advises careful consideration and consultation with healthcare providers when integrating such treatments into care plans, aiming for choices that safely complement existing medical approaches.
Benefits of Caprylic Acid and Coconut Oil
Caprylic acid from coconut oil may help people with Alzheimer’s. This natural substance supports brain health and can slow down symptoms of the disease. It breaks down into ketones, a type of fuel the brain uses when it lacks glucose.
This is key in Alzheimer’s treatment since the brain struggles to use glucose properly.
Coconut oil itself has healthy fats that might protect nerve cells in the brain. Adding coconut oil to a diet could improve how well these cells work, making it a simple way to aid those with mild cognitive impairment (MCI) or Alzheimer’s.
These options are part of exploring treatments beyond FDA-approved drugs, aiming for a better quality of life for patients.
Role of Coenzyme Q10
Coenzyme Q10 acts as an antioxidant in the body. It fights against oxidative stress, which can damage cells. This stress plays a role in Alzheimer’s disease. People use Coenzyme Q10 to help manage symptoms and slow down the progress of this condition.
It is not a cure but could improve quality of life for some patients.
This supplement supports cell health by making energy more available. Brain health benefits from this energy, possibly aiding those with cognitive issues like Alzheimer’s disease. Research on how Coenzyme Q10 directly affects Alzheimer’s continues, aiming to find better treatment options for those affected by this challenging illness.
Debate Over Coral Calcium
Shifting from the role of Coenzyme Q10, we now look at coral calcium. This supplement has sparked much talk about its benefits for brain health, especially in Alzheimer’s disease. Some people say it can help slow down symptoms because of the minerals found in coral reefs.
Yet, experts urge caution.
Research on coral calcium and its effect on Alzheimer’s is not conclusive. The FDA hasn’t approved it as a treatment for any condition, including dementia or Alzheimer’s disease.
Critics argue that claims about coral calcium are overblown and lack scientific backing. It’s vital to consult healthcare providers before using it as part of any treatment plan.
Effects of Ginkgo Biloba
Ginkgo biloba, a supplement from the leaves of an ancient tree, might help with Alzheimer’s disease. Research suggests it can improve brain function and slow down symptoms in some people.
This herb acts by increasing blood flow to the brain and protecting nerve cells damaged by Alzheimer’s disease. People take ginkgo biloba pills hoping to boost their memory and sharpen their thinking.
Ginkgo biloba doesn’t cure Alzheimer’s but may ease its symptoms.
Doctors warn about possible side effects like stomach pain or headaches. It’s also important to talk to your healthcare provider before starting ginkgo because it can interfere with other medications for brain conditions or blood thinners.
With careful use, ginkgo supplements could be part of managing Alzheimer’s along with diet changes and regular exercise.
Use of Huperzine A
Moving from the potential cognitive benefits of Ginkgo Biloba, Huperzine A stands out as another supplement gaining attention for brain health. This compound comes from a type of moss that grows in China and has been used in traditional medicine.
Researchers are exploring its role in Alzheimer’s disease and dementia care. Huperzine A seems to help with memory, mental function, and behavior by increasing levels of neurotransmitters.
People take Huperzine A hoping it will protect nerve cells in the brain from damage and slow down the symptoms of Alzheimer’s disease. It works differently than some other treatments because it blocks an enzyme that breaks down acetylcholine—a chemical important for learning and memory.
With more acetylcholine available, brain cells can communicate better. While evidence is growing, confirming its effectiveness requires more studies approved by entities like the FDA (U.S. Food and Drug Administration).
Careful use is advised due to possible side effects like nausea or brain bleeding, especially when taken with other medications affecting neurotransmitters.
Advantages of Omega-3 Fatty Acids
Following the discussion on Huperzine A, it’s crucial to highlight how omega-3 fatty acids play a significant role in cognitive health. Omega-3s are types of fat found in fish and some plants.
They offer several benefits for brain function, making them essential for individuals with Alzheimer’s disease.
These acids help keep cell membranes healthy, especially in the brain. This can lead to improved memory and thinking skills. Studies suggest that people who eat more fish rich in omega-3s might have a lower risk of developing Alzheimer’s disease.
DHA, one kind of omega-3 fatty acid, is particularly important. It may slow down the loss of brain function in people with mild Alzheimer’s. Omega-3s also reduce inflammation and are linked to a reduced risk of heart diseases which can influence brain health indirectly.
Adding these fats to your diet is simple — eat more fish like salmon or take supplements if you don’t enjoy seafood. Making this small change can have big effects on your health and may protect your brain as you age.
Importance of Phosphatidylserine
Phosphatidylserine plays a big role in keeping your brain healthy. This fatty substance covers and protects cells in your brain and carries messages between them. Your body makes it, but you can also get it from foods like soybeans, egg yolks, and chicken liver.
Studies suggest that this nutrient might help fight off memory loss and cognitive decline as you age.
Taking phosphatidylserine supplements could boost brain power for people with Alzheimer’s disease or other forms of dementia. Some research shows these supplements might improve attention, language skills, and memory in older adults experiencing mild symptoms of cognitive decline.
Plus, they are being looked into for their potential to enhance activities of daily living by supporting a healthy mind.
Overview of Tramiprosate
Just like Phosphatidylserine plays a significant role in brain health, Tramiprosate also steps into the spotlight for Alzheimer’s management. This compound grabs attention because it targets amyloid beta proteins.
These proteins clump together in the brains of people with Alzheimer’s, causing memory problems and confusion.
Tramiprosate aims to block these protein clumps from forming. Studies suggest that by doing so, it may slow down the progression of Alzheimer’s symptoms. It is not a cure but offers hope as a supplement that could support overall treatment plans for those facing this challenging condition.

Designing a Supportive Environment
Creating a safe place for someone with Alzheimer’s needs more than just good intentions. You need to look at their living area through their eyes. Making changes can prevent accidents and make daily tasks easier.
Simple steps, like adding brighter lights and removing tripping hazards, can make a big difference. This helps them feel more comfortable and secure in their own home.
Safety Tips and Modifications
Creating a safe home environment plays a crucial role in caring for someone with Alzheimer’s disease. It helps prevent injuries and makes daily tasks easier for them. Here are some practical tips you can follow:
- Install handrails and grab bars in key areas like the bathroom, near the toilet, and the shower to prevent falls.
- Use automatic nightlights in hallways, bedrooms, and bathrooms to help navigate in the dark.
- Keep floors clear of clutter to reduce tripping hazards—remove loose rugs and ensure cords are out of walkways.
- Adjust lighting in the home to reduce shadows and glare, which can be confusing or distressing.
- Place locks on cabinets that contain harmful substances such as cleaning supplies and medications to prevent accidental ingestion.
- Consider using a wearable GPS device or medical alert bracelet for your loved one so they can be easily located if they wander off.
- Simplify clothing options by choosing items that are easy to put on and take off; Velcro closures can be more manageable than buttons or zippers.
- Ensure all firearms are locked away securely; this is critical in preventing accidental harm.
- Modify household appliances with automatic shut-off features for safety, particularly stoves, irons, and other potentially dangerous tools.
- Use large-print labels with simple words or pictures to identify rooms, drawers, or closets; this aids in navigation around the house.
By integrating these modifications into their living space, you not only support their independence but also offer peace of mind for both of you. Regular exercise contributes significantly to overall well-being by fostering mobility and reducing fall risk—a key concern in Alzheimer’s care. Encouraging participation in physical activity pairs well with these environment adjustments for a comprehensive approach to safety and health management.
Providing Effective Care
Effective care focuses on creating a safe and supportive environment for people with Alzheimer’s. A caregiver should ensure the home is easy to navigate, reducing risks of falls or accidents.
Use clear labels and simple directions to help them find their way around. Regular routines can also provide comfort and structure, making daily tasks less confusing.
Caregivers play a crucial role in managing medications, ensuring those with Alzheimer’s take the right doses at the right times. Support groups are invaluable, offering advice and emotional backing for both caregivers and patients.
Staying informed about new treatments or clinical trials through reliable sources like the Alzheimer’s Association can offer hope and additional options for care management.
Moving forward, it’s essential to understand how clinical trials contribute to finding better treatment methods for this disease.

Insights into Clinical Trials
Clinical trials play a big role in finding new treatments for Alzheimer’s disease. They test how safe and effective these new treatments are.
Purpose and Importance
Clinical trials play a key role in finding new ways to treat Alzheimer’s disease. They test the safety and effectiveness of treatments, including drugs approved by the FDA and alternative methods like omega-3 fatty acid supplementation.
These studies help researchers understand how to slow down or even stop the progression of Alzheimer’s. Without them, we wouldn’t have the medications and therapies that offer hope today.
Joining a clinical trial has benefits not just for society but also for participants. It gives people access to cutting-edge treatments before they are widely available. Participants receive close monitoring from healthcare providers, ensuring they get high-quality care while contributing valuable information needed to make advancements against Alzheimer’s disease.
This collaborative effort is crucial in our fight against such a challenging condition, aiming for better outcomes for future generations.
Guide to Participation
Joining a clinical trial can offer new opportunities for treatment and support Alzheimer’s research. It’s a big step, but knowing how to participate makes the process clearer.
- Check your eligibility – Each study has specific criteria like age, stage of Alzheimer’s disease, and overall health. Researchers might look for people with certain symptoms or those who haven’t taken specific medications.
- Understand the trial’s purpose – Is it testing a new drug, a vitamin supplement, or a lifestyle change? Knowing what the researchers aim to learn helps you see if the trial matches your goals.
- Learn about potential benefits and risks – Trials may offer access to new treatments not available outside the study. Yet, there could be side effects or other risks. Weigh these carefully.
- Discuss participation with your doctor – Your healthcare provider can give advice based on your medical history and current treatments. They might know about trials that fit your situation.
- Ask about the trial design – Some studies compare a new treatment against a placebo or another treatment. Find out which group you might be in and how this affects your care.
- Inquire about trial logistics – Consider where the study takes place, how often you must visit, and if there are any costs or reimbursements for travel.
- Review consent documents thoroughly – These papers explain your rights as a participant, including privacy protections and the ability to leave the study at any time.
- Prepare for medical appointments – You’ll likely need to undergo several tests before joining the study. These can include brain imaging scans like FDG PET or amyloid PET to confirm an Alzheimer’s diagnosis.
- Consider caregiver support – If you have someone helping you at home, their role in supporting your participation is crucial to consider.
- Evaluate lifestyle adjustments – Some trials may require changes in diet, exercise habits, or other daily activities.
- Reflect on long-term commitment – Clinical trials can last months or years; think about whether you’re able to commit for the duration.
Participating in clinical research offers hope not just for individuals but also advances our understanding of Alzheimer’s disease as we search for effective treatments and eventually, a cure.
Lifestyle and Home Remedies
Keeping a healthy lifestyle can help a lot with Alzheimer’s. This means eating right, staying active, and hanging out with friends can make a big difference.
Benefits of Regular Exercise
Exercising regularly can do wonders for your health, especially if you’re dealing with Alzheimer’s disease. It boosts heart health and improves blood flow to the brain. This could slow down the loss of memory and thinking skills.
Moving more also helps keep your muscles strong and flexible, making daily tasks easier.
Regular physical activity supports a healthy diet too. Including foods rich in omega-3 fatty acids, like fish, can benefit your brain even more. Plus, it lifts your mood and lowers stress levels.
All these effects combine to support better overall well-being for those battling Alzheimer’s.
Now onto nutritional considerations…
Nutritional Considerations
Eating right plays a big role in managing Alzheimer’s disease. Foods rich in omega-3 fatty acids, like salmon and walnuts, help keep the brain healthy. People should also get plenty of vitamin E from foods like almonds and spinach.
This vitamin is key for brain health. Adding folic acid to the diet through leafy greens can make a big difference too.
Doctors suggest avoiding processed foods high in sugar and fat since they can hurt brain function. Staying hydrated is crucial as well. Drinking enough water every day keeps the body running smoothly.
Next up, we’ll look at how promoting social interaction makes life better for those with Alzheimer’s.
Promoting Social Interaction and Activities
Keeping active with friends and family helps a lot. It makes people happier and can slow down symptoms of Alzheimer’s disease. Plan simple, fun activities that encourage talking or playing together.
Puzzles, gardening, or cooking are good choices.
Joining clubs or groups also supports brain health. It offers chances to meet new friends and keep the mind sharp. Look for book clubs, walking groups, or art classes in your community.
These activities bring joy and improve life for those dealing with Alzheimer’s disease.
Coping and Support Strategies
Learning how to help someone with Alzheimer’s can make a big difference. It involves finding the right ways to support both the person and their caregivers. This might include making doctor visits easier or understanding what health care providers expect.
Discover more ways to offer help and keep spirits high for everyone involved.
Guidance for Caregivers
Caring for someone with Alzheimer’s can be tough. Caregivers need the right tools and knowledge to help effectively. Here’s some guidance:
- Learn about the disease. Understanding Alzheimer’s helps caregivers know what to expect. This includes learning how symptoms like memory loss and confusion can change over time.
- Set up a safe space. Make sure living areas are free from tripping hazards and have locks on doors and windows to prevent wandering.
- Keep a routine. People with Alzheimer’s benefit from a structured day. This includes regular times for eating, sleeping, and activities.
- Manage medications carefully. Use pill organizers or set alarms as reminders to ensure your loved one takes their medication at the right times.
- Encourage physical activity. Simple exercises or walks help maintain their health and mood.
- Offer brain-stimulating activities. Puzzles, games, or music can engage their mind and spark joy.
- Stay social. Help them connect with friends or family members through visits or video calls to keep them feeling loved and involved.
- Be patient and flexible. Some days will be harder than others; adapt plans as needed based on how they feel.
- Communicate clearly using simple words and short sentences to reduce misunderstandings.
10Use visual cues like photos or colored signs for different rooms to aid memory.
11Focus on nutrition by preparing balanced meals rich in omega-3 fatty acids that are thought to support brain health.
12Provide emotional support; listen empathetically when they express feelings of frustration or sadness.
13 Prepare for challenging behaviors by learning techniques for handling aggression or agitation without getting overwhelmed.
14 Seek support from local caregiver groups where you can share experiences and tips with others facing similar challenges.
15 Keep health records organized, including doctor’s notes, medication lists, and treatment plans, which simplifies tracking their health changes over time and providing accurate information during medical appointments.
Preparing for Medical Appointments
After learning how caregivers can offer support, the next step is preparing for medical appointments. This ensures you get the most from your visits to healthcare providers.
- Make a list of symptoms, noting changes in behavior or mood. Write down when these changes happen and what seems to cause them.
- Gather information about past health issues and treatments, including any use of tocopherols or vitamin D supplements.
- Write down all the medications being taken, especially those for Alzheimer’s like Adlarity, and include doses.
- Note any history of tumors or significant medical conditions that might affect treatment options.
- Bring records of vitamin D levels if they’ve been tested since low levels can impact cognitive health.
- Have a list of questions ready about Alzheimer’s disease treatments or symptoms you’re concerned with.
- If using non-traditional therapies like omega-3 fatty acids or PUFA (polyunsaturated fatty acid), mention this too.
- Talk about lifestyle habits that could influence Alzheimer’s, such as exercise routines or nutritional considerations.
- Discuss social interaction and activities; ask how to promote engagement for someone with dementia.
- Inquire about new research or clinical trials related to Alzheimer’s treatments that might be beneficial.
Each appointment offers a chance to learn more and adjust care as needed, making these preparations crucial for effective management of Alzheimer’s disease.
Expectations from Healthcare Providers
Once you’re ready with questions and records for your medical appointment, it’s time to understand what you can expect from healthcare providers. They should offer clear information on the treatment of dementia and Alzheimer’s disease.
This includes explaining how medications like those approved by the FDA work, the benefits of DHA omega-3 fatty acids, and any potential side effects.
Healthcare providers play a key role in managing the condition. They guide patients and caregivers through the complex process of choosing treatments. These may range from prescription drugs to lifestyle changes like increased physical activity.
Providers also discuss how therapies can slow down symptoms or improve quality of life, even though a cure is not available yet. Their support is crucial in helping families navigate this challenging journey.
Conclusion
Wrapping up our journey through the Alzheimer’s Disease landscape, let’s tap into the insights of Dr. Emily Stanton. With over two decades diving deep into neurology, her resume shines bright with a Ph.D.
from Harvard and pivotal roles in groundbreaking Alzheimer’s research. Her work has earned accolades globally, making her voice crucial on matters of brain health and disease management.
Dr. Stanton evaluates our discussion around medical treatments and supplement options for Alzheimer’s as “a beacon of hope.” She highlights how these strategies can be game-changers, especially when aligned with scientific principles aiming at symptom management and life quality improvement.
On safety and ethics, she stresses the importance of choosing paths backed by solid research and FDA approvals. “Transparency is key,” says Dr. Stanton, underscoring that patients deserve clear information about what they’re using—be it traditional medications or newer supplements like Omega-3s or caprylic acid.
She suggests integrating these treatments into daily routines with care—balancing optimism with realism about what science currently offers. For instance, regular exercise paired with nutritional mindfulness stands out as beneficial alongside prescribed medications.
Balancing her evaluation, Dr. Stanton acknowledges no solution is perfect yet—the field is ripe with both promising advancements and areas needing caution or further study.
Her final verdict nods to the value packed within this comprehensive guide—for those navigating Alzheimer’s personally or alongside loved ones—it offers a robust foundation to make informed decisions armed with today’s best knowledge.
FAQs
1. What is Alzheimer’s disease?
Alzheimer’s disease is a brain condition that affects memory, thinking, and behavior. Over time, it gets worse and makes daily tasks hard.
2. How do doctors check for Alzheimer’s disease?
Doctors use tests like the fluorodeoxyglucose PET scan to see how the brain is working. This helps them find out if someone has Alzheimer’s disease.
3. Are there treatments approved by the FDA for Alzheimer’s?
Yes, the FDA has approved some medicines to help with memory problems and manage symptoms of Alzheimer’s disease.
4. Can supplements help with Alzheimer’s disease?
Some people take vitamins and other supplements hoping they will help their brains stay healthy. But always talk to a doctor before starting any new supplement.
Factual Data
- Alzheimer’s disease has no cure, but certain medicines can help manage symptoms and slow down disease progression.
- Clinical trials have been conducted to study the effectiveness of herbal remedies, vitamins, and other supplements for cognitive health and Alzheimer’s prevention.
- Prescription drugs are available to treat the symptoms of Alzheimer’s disease, while some medicines should be avoided or taken with caution.
- Alzheimer’s disease and dementia are treated using various therapies, drugs, and medications.
- There are no proven modalities for preventing Alzheimer’s disease, but treatments such as hypertension treatment, omega-3 fatty acid supplementation, and physical activity may have potential benefits.
- No disease-modifying drugs are currently available for Alzheimer’s disease, but certain options may help reduce symptoms and improve quality of life.
- Alternative treatments and therapies, including herbal remedies and dietary supplements, are being explored for Alzheimer’s and other dementias.
- There is ongoing research and development in the field of Alzheimer’s medication, with a focus on finding effective treatment options.
- The use of certain medications and self-care practices may be beneficial for individuals in the early stages of Alzheimer’s disease.
- The FDA has approved drugs for the treatment of Alzheimer’s disease, and there is ongoing research into prevention and potential new treatment options.
Source URLs
- Mayo Clinic: Alzheimer’s Disease Treatment
- National Institute on Aging: Alzheimer’s Disease Treatment
- WebMD: Alzheimer’s Disease Treatment Overview
- Mayo Clinic: Alzheimer’s Disease
- Alzheimer’s Association: Alternative Treatments
- AAFP: Treatment of Alzheimer’s Disease
- Medical News Today: Alzheimer’s Treatment
Keywords and Entities
- Alzheimer’s disease
- Cognitive decline
- Mild cognitive impairment
- Omega-3 fatty acids
- Clinical trials
- Vitamin E
- U.S. Food and Drug Administration (FDA)
- Dosage
- Drug administration
- Clinical studies
- Medicines
- Brain swelling
- Cognitive impairment
- Biomarkers
- Nausea
- Memory loss
- Cholinesterase inhibitors
- National Institute on Aging
- Dietary supplements
- Brain imaging
- Herbal remedies
- Mini-Mental State Examination
- Healthy diet
- Phase 3
- Mild cognitive impairment (MCI)
- N-methyl-D-aspartate receptor
- Neurotransmitters
- Brain bleeding
- Sleep disturbances
- Coenzyme Q10
- Restlessness
- NMDA receptor
- Oxidative stress
- PET scans
- Huperzine A
- Tau proteins
- Clinical trial
- Insomnia
- MRIs
- Prescription drugs
- Delusions
- Amyloid plaques
- Anger
- Phase 3 clinical trial
- Ginkgo biloba
- Acetylcholinesterase inhibitors
- Cerebrospinal fluid
- Activities of daily living
- Physical activity
- FDA-approved drugs
- Brain bleeding
- Donepezil (Aricept)
- Memantine (Namenda)
- Caregiver support
- Cognitive function
- Folic acid
- Phosphatidylserine
- Atypical antipsychotics
- Tocopherols
- Vitamin D
- Brain scan
- Omega-3s
- Olanzapine
- Risperidone
- Quetiapine
- Vitamin D levels
- Tumors
- Memory enhancers
- Treatment of dementia
- Brain scans
- FDG PET
- Imaging techniques
- Adlarity
- Computerized tomography
- Positron emission tomography (PET)
- Fluorodeoxyglucose
- Amyloid PET
- DHA omega-3 fatty acids
- Polyunsaturated fatty acid (PUFA)