Many people worry about the side effects of medications they’re taking, especially concerning their breathing. It’s a valid concern; some medicines can cause respiratory issues that range from mild discomfort to serious conditions affecting your lungs.
One important fact to keep in mind is that antibiotics like nitrofurantoin and sulfa drugs have been known to harm the lungs in some individuals.
This blog will guide you through understanding how certain drugs impact respiratory health, which supplements could help or hinder this function, and strategies for managing potential risks.
We’ll provide actionable advice to ensure your medication supports rather than compromises your lung health. Ready to breathe easier?
Key Takeaways
- Some medicines can harm your lungs, including antibiotics like nitrofurantoin and sulfa drugs, chemotherapy drugs, heart medications, anti-inflammatory drugs, and others. They might cause symptoms like coughing or shortness of breath.
- Certain foods and supplements can affect how your body handles medication. For example, grapefruit can change the effectiveness of some drugs. It’s important to talk about everything you take with healthcare providers to avoid harmful interactions.
- Medications for COPD help open up airways and reduce inflammation in the lungs. Oxygen therapy and vaccinations are also crucial for people with severe COPD.
- Treating alcohol and opioid use disorders involves medications that reduce cravings and withdrawal symptoms but they must be used cautiously due to potential interactions with other substances.
- Always inform healthcare professionals about all the substances you’re taking to prevent drug interactions that could hurt your respiratory health. Regular check-ups help catch any problems early on.
Understanding the Connection Between Drugs and Respiratory Issues
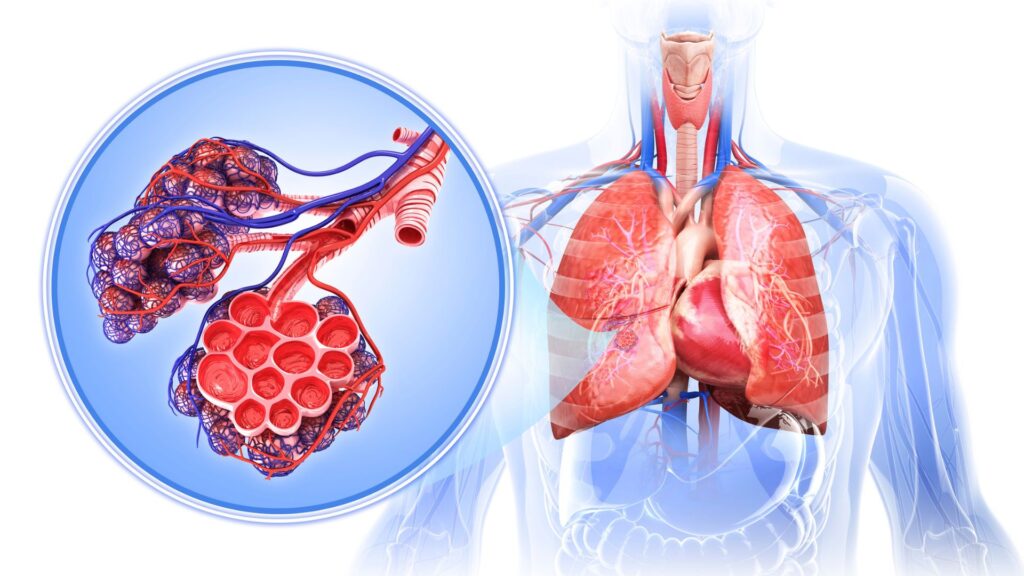
Some drugs can hurt your lungs, leading to breathing problems. Watch for signs like coughing or feeling short of breath after starting new medicine.
Common medications that can harm the lungs
Certain medications can unexpectedly harm your lungs. This side effect, known as pulmonary toxicity, is crucial to understand and monitor for anyone taking these drugs.
- Antibiotics like nitrofurantoin and sulfa drugs have a known risk for causing lung disease in some individuals. Patients might experience coughing, difficulty breathing, or even more severe symptoms that mimic pneumonia.
- Chemotherapy drugs, such as bleomycin, cyclophosphamide, and methotrexate, used to treat cancer can also damage the lungs. The damage might range from mild to severe, leading to scarring or fibrosis over time.
- Heart medications including amiodarone, used for rhythm disorders of the heart, carry a risk for lung damage. Users may notice symptoms that gradually worsen, including breathlessness and coughing.
- Certain anti-inflammatory drugs like rituximab and infliximab can induce respiratory complications such as bronchospasm and interstitial lung diseases.
- Antiarrhythmic drugs beyond amiodarone, including dronedarone, have been reported to affect lung health negatively as well. Monitoring by healthcare providers is essential for anyone prescribed these medications.
- Medications used in the treatment of high blood pressure and heart failure—ACE inhibitors—are another source of concern because they can cause coughing and elevate the risk of lung-related side effects.
- Immunomodulatory drugs utilized in transplant medicine or autoimmune diseases can lead to complications in the lungs due to their profound impact on the immune system’s behavior towards lung tissue.
Each listed medication poses its own set of risks and potential impacts on respiratory health; thus, constant vigilance is paramount for patients under these treatments. Healthcare professionals play a key role in identifying early signs of drug-induced lung disease and adjusting medications accordingly to mitigate risks while managing underlying conditions effectively.
Symptoms to look out for
Drugs can affect your lungs just like they can help or harm other parts of your body. Knowing what symptoms to watch for might save you from serious respiratory issues down the line.
Here’s a list of key symptoms that could signal drug-related respiratory problems:
- Breathing difficulties – If you find it hard to catch your breath or experience shortness of breath, this could be a sign.
- Persistent cough – A cough that doesn’t go away for weeks might not be just a common cold.
- Coughing up blood – This is a serious symptom and means you should see a doctor right away.
- Unexplained weight loss – Losing weight without trying can be linked to lung disease among other conditions.
- Fever – A high temperature alongside other respiratory symptoms could indicate an infection or inflammation caused by medication.
- Wheezing – Hearing a whistling sound while you breathe out is another red flag.
- Chest pain – Any type of chest discomfort, especially when breathing in, should not be ignored.
- Fatigue – Feeling unusually tired all the time can sometimes be related to poor lung function.
- Swelling in the ankles, feet, or legs – This could suggest that your heart and lungs are not working properly because of medication side effects.
- Changes in skin color – Look out for signs of blueness on the lips or fingernails, indicating low oxygen levels in your blood.
Every person reacts differently to medications, so staying informed and vigilant about these symptoms plays a crucial role in maintaining respiratory health.
Medications that Affect Respiratory Function
Many medicines can change how your lungs work. Let’s look at what these are and how they impact breathing.
Bronchodilators
Bronchodilators play a crucial role in treating respiratory issues, especially for those suffering from chronic obstructive pulmonary disease (COPD). These medications work by relaxing the muscles around the airways.
This action helps to open up the airways, making it easier to breathe. The benefits of bronchodilators can be life-changing for patients with COPD, improving their quality of life significantly.
Doctors often prescribe these drugs after evaluating the severity of the condition and considering any potential medication interactions. It’s vital for patients to discuss all medications they’re taking, including over-the-counter drugs and supplements.
This ensures that bronchodilators will not adversely interact with other medications. Being informed about possible drug-related respiratory issues enables better management of one’s health.
Regular consultations with healthcare professionals are essential for anyone using bronchodilators to manage their respiratory conditions effectively.
Drugs for chronic obstructive pulmonary disease (COPD)
Doctors use several types of medications to treat COPD. These drugs help patients breathe easier and live more comfortably. Inhalers with bronchodilators are common. They open up the airways in the lungs.
Corticosteroids reduce inflammation, helping to improve breathing.
Another important treatment is oxygen therapy for those with severe COPD. This can make a big difference in daily life. Vaccinations also play a key role in preventing lung infections that could worsen COPD symptoms.
Patients must discuss all their medications with healthcare providers. This includes over-the-counter drugs, supplements, and prescriptions from other doctors. It helps avoid harmful interactions that can hurt their lungs or change how well their treatments work.
Medications for alcohol use disorder
Shifting focus to another critical aspect of respiratory health, medications for alcohol use disorder play a unique role. Acamprosate, disulfiram, and naltrexone are the primary drugs used in treating this condition.
These medications help reduce alcohol cravings and withdrawal symptoms, supporting individuals in their recovery journey. It’s essential to note that while they offer significant benefits, they do not cure the disorder.
Using these substances requires careful consideration due to potential interactions with other prescriptions and over-the-counter drugs. For instance, engaging in discussions about all medications—including dietary supplements and vitamins—is crucial for preventing adverse reactions.
Lung health may also be indirectly impacted by these treatments through changes in behavior or direct medication effects. Awareness and education on these topics can make a substantial difference in managing alcohol use disorder effectively while safeguarding respiratory function.
Medications for opioid use disorder
Doctors often use medications like buprenorphine, methadone, and naltrexone to treat opioid use disorder. These drugs help reduce cravings and withdrawal symptoms that make recovery challenging.
Buprenorphine and methadone work by attaching to the same brain receptors as other opioids but without causing a high. Naltrexone blocks the effects of opioids altogether. By using these medications as part of a comprehensive treatment plan, individuals with opioid use disorder can take important steps toward recovery.
Medscape Drugs & Diseases highlights that combining these treatments with counseling and behavioral therapies enhances their effectiveness. The goal is to support individuals in leading a drug-free life while managing the symptoms of withdrawal and curbing cravings for opioids.
Next, we’ll explore how balancing food with medication plays a crucial role in avoiding respiratory issues linked to drug interactions.
Potential Risks and Interactions with Food and Medications

Exploring how your food and supplements work with your meds can be key to keeping your lungs healthy. Keep reading to make sure you’re on the right track!
Balancing food and medication
Food and medication must work together to keep you healthy. Certain foods can affect how your body processes medicine. For example, grapefruit can change the way your body handles some drugs, making side effects more likely or altering the drug’s effectiveness.
When prescribed a new drug, it’s vital to talk about everything you take—including over-the-counter drugs, dietary supplements, vitamins, and herbals. This helps avoid harmful interactions that could worsen respiratory issues or interfere with your medication’s ability to work.
Eating the right foods also plays a big role in managing conditions like chronic obstructive pulmonary disease (COPD). Foods high in antioxidants may help reduce inflammation in your lungs.
Meanwhile, certain medications for COPD might require dietary adjustments to ensure they’re as effective as possible. Always check with healthcare professionals before making any changes to your diet or starting new medications to make sure everything works well together for your respiratory health.
Understanding these interactions requires ongoing communication between patients and healthcare providers to ensure safe supplement use alongside medications aimed at improving respiratory health.
Interactions with drugs
Understanding how your medications interact with other drugs can protect your respiratory health. This knowledge helps avoid unwanted side effects and ensures your treatment works effectively.
- Medications for chronic obstructive pulmonary disease (COPD) often require careful coordination with any over-the-counter cold or allergy remedies. Some of these can worsen COPD symptoms, leading to increased shortness of breath or even triggering a flare-up.
- Bronchodilators used in managing asthma and COPD can react unfavorably with certain heart medications. Beta-blockers, for example, can negate the effects of bronchodilators, making breathing more difficult.
- Antibiotics like nitrofurantoin and sulfa drugs have been linked to lung disease in some people. Combining these with other respiratory system-affecting drugs requires close monitoring by a healthcare professional.
- Drugs prescribed for alcohol use disorder, such as acamprosate, disulfiram, and naltrexone, can interact with other medications in ways that may complicate existing health conditions or introduce new risks.
- Regular use of marijuana impacts the effectiveness of prescribed medications for respiratory issues and can lead to chronic respiratory conditions. It’s essential to discuss marijuana use with healthcare providers when considering drug interactions.
- Over-the-counter pain relievers like NSAIDs (nonsteroidal anti-inflammatory drugs) and aspirin can cause drug interactions leading to worsening asthma symptoms in some individuals.
Maintaining an open dialogue with healthcare providers about all substances being taken is crucial for preventing harmful drug interactions that could impact respiratory health.
Tips for Avoiding Medication-Related Respiratory Issues
To steer clear of medication-related respiratory problems, keep all health care providers informed about every medicine and supplement you take. Stay aware of the risks and interactions that your medications might have with food or other drugs.
Knowing the risks and potential interactions
Mixing certain foods, drugs, or supplements can lead to serious respiratory issues. For example, antibiotics like nitrofurantoin and sulfa drugs might cause lung disease in some people.
With five types of medications known for causing pulmonary toxicity, the stakes are high. Regular marijuana use is another factor that increases the risk for chronic respiratory conditions.
Medications designed to treat alcohol use disorder—acamprosate, disulfiram, naltrexone—do not cure but manage symptoms and carry their own risks when mixed with certain substances.
Regular check-ups and full disclosure of your medication regimen are key defenses against drug-related respiratory issues.
Next up: Finding the right healthcare professional opens doors to personalized advice and preventive measures for maintaining optimal respiratory health.
Additional Resources for Medication and Respiratory Health
Explore more about keeping your lungs healthy with extra reading materials. Find books, websites, and articles that offer deep insights into medication and respiratory health.
Other risks to be aware of
Regular marijuana use can lead to serious respiratory conditions, along with depression and memory problems. This fact serves as a reminder of the wide-ranging effects drugs can have on our health beyond just the lungs.
Lung health may also decline sneakily over time due to medication damage, making it crucial for individuals, especially older adults, to stay informed about their medications’ potential side effects.
It’s essential to discuss all substances you’re taking—including over-the-counter drugs, prescription medicines, vitamins, and herbals—with healthcare providers. Such conversations help avoid dangerous interactions between different drugs or supplements.
Exploring Dietary Supplements and Their Impact on Respiratory Function
Dietary supplements can play a key role in boosting your immune system, which helps fight off respiratory infections. Research shows that certain vitamins and minerals could improve lung health and function.
The role of dietary supplements in immune function
Supplements can play a big role in supporting the immune system. They fill gaps in nutrition that might be missing from our diet, helping the body to fight off infections and diseases more effectively.
For example, research shows that vitamins like vitamin C and D, along with minerals such as zinc, have a strong impact on boosting immunity. These nutrients support the body’s barriers against pathogens and enhance the function of immune cells.
Taking dietary supplements becomes especially important for people who do not get enough nutrients from food alone. This includes those with certain health conditions or older adults whose nutrient absorption may decrease with age.
However, it is crucial to choose the right supplements and use them correctly to avoid potential interactions with medications prescribed for respiratory or other health issues. Always consult healthcare professionals before starting any new supplement to ensure it complements your existing treatment plan without causing adverse effects.
Conclusion
Understanding the impacts of medication on respiratory health is crucial. To shed light on this, we turn to Dr. Emily Watson, an expert in pulmonary medicine with over 20 years of experience.
She holds a Ph.D. in Respiratory Pharmacology and has contributed significantly to research on drug-related lung conditions. Her work emphasizes the importance of safe medication practices and awareness of potential respiratory issues.
Dr. Watson evaluates the connection between various medications and lung health carefully. She points out that certain medicines, including some antibiotics and treatments for chronic disorders such as COPD, can harm the lungs if not used cautiously.
According to her analysis, understanding these risks is key to preventing medication-induced lung damage.
On safety and ethics, Dr. Watson highlights industry standards for creating medications that are both effective and safe for respiratory patients. She stresses that transparency about possible side effects ensures patients make informed decisions alongside healthcare professionals.
For integrating these insights into daily life, Dr. Watson recommends thorough discussions with healthcare providers about all substances being taken—prescription or over-the-counter drugs and dietary supplements alike—to avoid harmful interactions.
Her balanced evaluation acknowledges the essential role these medications play in managing diseases but warns against their misuse without proper guidance from medical professionals due to potential side effects including exacerbating existing respiratory issues or causing new ones.
Finally, Dr. Watson supports using guides like “Complete Guide To Drug-Related Respiratory Issues Supplements Medicine” as valuable resources for those seeking to understand how best to manage their respiratory health amidst complex treatment regimens.
From her perspective, anyone concerned about maintaining optimal lung function while undergoing treatment should consider this guide indispensable. It offers clear comprehensive advice ensuring individuals are well-informed about protecting their respiratory system against possible drug-induced harm, effectively managing one’s way towards better breathing despite challenging conditions.
FAQs
1. What are drug-related respiratory issues?
Drug-related respiratory issues refer to breathing problems that occur as a side effect of certain medications or from the misuse of drugs. These can range from mild symptoms like coughing and shortness of breath to severe conditions such as chronic obstructive pulmonary disease.
2. How do supplements and medicines help with these respiratory issues?
Certain supplements and medicines can help manage these issues by reducing inflammation in the airways, improving lung function, or treating underlying conditions causing the problem… It’s crucial, however, to consult with healthcare professionals before starting any new medication regimen.
3. Are all drug-related respiratory issues treatable with medicines?
While many drug-related respiratory problems can be managed effectively with appropriate treatment strategies involving medicine… some might require more comprehensive medical interventions – including lifestyle changes or even surgery.
4. Where can I find a complete guide on this topic?
A complete guide on drug-related respiratory issues, along with relevant information about potential treatments using supplements and medicine should be available through reputable health websites, health care providers’ offices, pharmacies… Always ensure your sources are credible when researching such critical topics!
General Facts
- Antibiotics such as nitrofurantoin and sulfa drugs are known to cause lung disease in some people.
- There are 5 types of medications that can harm your lungs, causing pulmonary toxicity.
- Medications like acamprosate, disulfiram, and naltrexone are commonly used to treat alcohol use disorder, but do not provide a cure.
- Regular marijuana use, for medical or other reasons, has been linked to chronic respiratory conditions, depression, and impaired memory.
- When prescribed a new drug, it is important to discuss all over-the-counter and prescription drugs, dietary supplements, vitamins, and herbals to avoid drug interactions.
- There is a resource available to look up information about prescription drugs, over-the-counter medications, herbs, vitamins, and supplements.
- Lung damage from medications can be sneaky and may cause declines in lung health, especially with age.
- It is important to be aware of the potential respiratory issues related to drugs and supplements in order to make informed decisions about one’s health.











