Addressing liver cirrhosis can seem challenging. You might be concerned about your health, curious about treatment opportunities, and exploring ways to enhance your condition through diet or supplementary means.
With an abundance of information available, it can be challenging to identify what will genuinely assist you. A fundamental truth is evident: amendments in lifestyle and the right medication can considerably control cirrhosis and avert further liver injury.
This article serves as a comprehensive manual on liver cirrhosis — encapsulating all aspects from its causes, symptoms, and phases to in-depth suggestions on treatments, inclusive of medications and supplements that might prove beneficial to you.
We’ll also explore guidelines related to nutrition that are planned to uphold your liver’s health. Prepared to reclaim your power? Continue reading.
Key Takeaways
- Cirrhosis turns healthy liver tissue into scar tissue, stopping the liver from working well. It can come from alcohol use, fat buildup in the liver, damaged bile ducts, or inflammation.
- To fight cirrhosis, doctors suggest lifestyle changes like no alcohol and more exercise. They also prescribe medicines such as acamprosate and naltrexone for alcohol-related damage. Herbal supplements like milk thistle might help but are still being studied.
- People with cirrhosis should eat smaller meals that have more calories and protein but less salt to help manage symptoms like fluid retention.
- A liver transplant may be needed when cirrhosis leads to liver failure. This is a big surgery where a sick liver is replaced with a healthy one.
- Keeping up with doctor visits and testing helps track the health of your liver. This way, doctors can make sure you’re getting the right treatment to live better with cirrhosis.
Exploring Cirrhosis
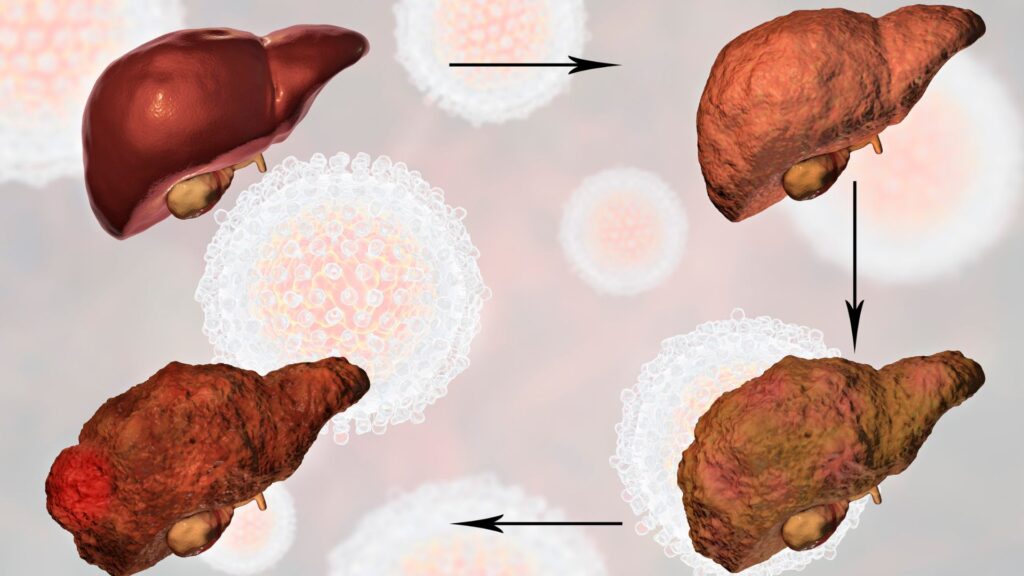
Cirrhosis turns healthy liver tissue into scar tissue, stopping the liver from working well. This condition can come from many causes and has different types to watch out for.
Definition and Types
The liver, a vital organ, can fall victim to cirrhosis, a disease marked by scarring and impaired function. This condition manifests in various forms, including alcoholic cirrhosis caused by excessive alcohol use and nonalcoholic steatohepatitis (NASH), stemming from fat buildup in the liver.
Other types include biliary cirrhosis, resulting from damaged bile ducts, and autoimmune hepatitis leading to liver inflammation.
Understanding the basics of liver health and cirrhosis is crucial for managing this condition.
Each type poses its unique risks but shares a common outcome: the gradual worsening of liver function over time. Prescribed medicines like acamprosate and naltrexone can address alcohol-induced damage while lifestyle changes counteract other causes.
Despite uncertainties surrounding their effectiveness, herbal supplements such as milk thistle are often explored for potential benefits.
Symptoms
The liver manifests numerous signals to indicate that something is not right in the body when one has cirrhosis. Prompt recognition of these symptoms can expedite diagnosis and the formulation of a treatment plan. Here is an in-depth exploration of the usual signs that suggest cirrhosis:
- The yellowing of the skin and eyes, a condition called jaundice, arises when the liver isn’t able to adequately filter bilirubin.
- Constant fatigue sets in, not just from lack of sleep, but due to a buildup of toxins in your blood that zap your energy.
- Swelling in the legs and abdomen happens due to fluid retention, a status often linked to liver damage.
- If you’re bruising and bleeding more easily than normal, it’s a hint that the liver is having difficulty making the proteins necessary for blood clotting.
- Itchy skin is another typical sign; the accumulation of bile salts under the skin due to improper bile flow results in persistent itching.
- A loss of appetite that leads to weight loss as cirrhosis advances, makes food seem less desirable.
- Nausea or vomiting can show up due to a strained digestive system that’s having trouble removing toxins.
- Confusion or difficulty thinking clearly are signs pointing to hepatic encephalopathy, a condition where toxin levels elevate in the brain due to liver failure.
- Spider-like blood vessels become noticeable on the skin’s surface; these are small, spider-shaped capillaries that result from hormone imbalances associated with liver disease.
- Long-term cirrhosis patients may have weak bones due to insufficient absorption of nutrients like calcium.
Each of these symptoms demonstrates the crucial role the liver plays in our health, and emphasizes that early detection can bring about substantial improvements in the treatment results for those struggling with cirrhosis.
Causes and Risk Factors
Liver cirrhosis develops for many reasons. Alcohol use stands out as a major cause, with medicines like acamprosate and naltrexone often prescribed to manage alcohol dependence. Yet, the condition isn’t limited to those who consume excessive alcohol.
Hepatitis infections, fatty liver disease tied to obesity and diabetes, and blockages in the bile ducts also play significant roles in causing this damaging liver scarring. Patients struggling with cirrhosis face an elevated risk of serious health complications—liver failure and an increased chance of liver cancer are among the dire possibilities.
Lifestyle choices significantly impact one’s risk factors for developing cirrhosis; thus, adopting healthy habits is crucial in prevention efforts. Regular exercise, monitoring medication safety due to altered drug processing by a damaged liver, and ensuring adequate intake of vitamins and minerals can all support liver health.
Spotting these causes early helps tailor treatments such as lifestyle changes or medications more effectively. Next up: understanding how doctors diagnose and stage this serious condition.
Diagnosing and Staging Cirrhosis
Doctors use several tests to diagnose cirrhosis and determine its stage. This step is crucial for deciding on the best treatment plan.
Diagnostic Tests
Diagnosing cirrhosis early is key to effective treatment and preventing further liver damage. Medical professionals rely on a combination of tests to get a clear picture of liver health.

- Blood Tests – A series of blood tests, known as liver function tests, measure levels of enzymes and proteins in your blood. High levels can indicate liver damage or disease.
- Imaging Tests – Ultrasound, CT scans, and MRI are tools doctors use to look at the liver. These imaging tests can show liver size, signs of cirrhosis, and whether there’s any tumor present.
- Liver Biopsy – This involves taking a small sample of liver tissue with a needle. The tissue is then examined under a microscope to determine the extent of liver damage.
- FibroScan – Also called transient elastography, this non-invasive test uses sound waves to measure the stiffness of your liver. Stiffer livers usually mean more scar tissue from cirrhosis.
- Endoscopy – For checking varices (enlarged veins), an endoscope—a thin tube with a camera—is passed down your throat into your stomach. It helps find bleeding risks in people with cirrhosis.
- Albumin Test – Albumin is a protein made by the liver; low levels suggest poor liver function often seen in cirrhosis patients.
- Prothrombin Time (PT) – PT measures how long it takes for your blood to clot. Delayed clotting times can indicate liver issues since the organ produces proteins needed for clotting.
- Bilirubin Test – Increased levels of bilirubin in the blood may indicate that the liver isn’t processing waste products correctly, which is common in cirrhosis.
These diagnostic methods form the basis for understanding how advanced cirrhosis is and guide treatment options including lifestyle modifications, medications like acamprosate or naltrexone for alcohol-related causes, and potentially a liver transplant for severe cases.
The Four Stages of Cirrhosis
Understanding the progression of cirrhosis is crucial for patients and their healthcare providers to manage the condition effectively. The disease unfolds in four distinct stages, each with its own set of challenges and treatment requirements. We will explore these stages, outlined in the table below:
| Stage | Description | Key Characteristics |
|---|---|---|
| 1. Inflammation | The liver becomes inflamed, indicating the beginning of liver damage. | Mild liver damage with no fibrosis. |
| 2. Fibrosis | Scar tissue begins to form, replacing healthy liver tissue. | Increased liver damage, moderate fibrosis, but no complications. |
| 3. Compensated Cirrhosis | The liver is heavily scarred but can still perform most of its functions. | Significant fibrosis, potential for complications begins, liver function maintained. |
| 4. Decompensated Cirrhosis | The liver is severely damaged and unable to function properly. | Severe fibrosis, liver failure, and life-threatening complications. |
At every stage, lifestyle modifications, nutritional guidelines, and medication play a crucial role in managing cirrhosis. Specific treatments may include prescription medicines like acamprosate and naltrexone to reduce alcohol use, a major cause of liver damage. Supplements, although used by some to support liver health, such as milk thistle, have uncertain efficacy in treating cirrhosis according to current research.
Also, adjustments in diet are suggested to ensure patients with cirrhosis consume more calories and protein while reducing salt intake to fight fluid retention and bloating. Ensuring adequate intake of vitamins and minerals is essential to prevent further complications, such as osteoporosis, given that individuals with cirrhosis may have deficiencies in these areas.
Each stage of cirrhosis brings its potential complications, including liver failure, portal hypertension, and hepatic encephalopathy, marking the importance of regular medical check-ups to monitor the disease’s progression and adjust treatment plans as necessary. Active measures, including reducing alcohol consumption and participating in regular exercise, are critical in managing cirrhosis and maintaining liver health to the best extent possible.
Complications Associated with Cirrhosis
Cirrhosis can lead to serious health problems. These include liver failure and increased blood pressure in the liver vessels.
Liver Failure
Liver failure is a severe complication of cirrhosis, where the liver can’t perform its vital functions. This condition often results from years of battling liver disease and damage.
Liver failure signals that treatment options like lifestyle changes, medications, or even a liver transplant may be urgently needed to save a patient’s life. Medicines such as acamprosate and naltrexone help address issues like alcohol use, which is a common cause behind the scarring of the liver.
In this stage of cirrhosis, the importance of nutritional supplements and dietary recommendations becomes even more critical. Since patients with cirrhosis might be low in vitamins and minerals—risking further complications like osteoporosis—they must get enough nutrients through their diet supplemented by vitamins and minerals.
Ensuring proper nutrient intake helps manage symptoms and supports overall liver health.
Understanding cirrhosis and managing it early can prevent progression to liver failure—a condition demanding immediate action for survival.
Portal Hypertension
Moving beyond liver failure, we find that portal hypertension is another significant complication of cirrhosis. This condition happens when the normal flow of blood through the liver gets blocked by scar tissue.
As a result, pressure builds in the portal vein—this is the main vessel that carries blood from your digestive organs to your liver.
Portal hypertension can lead to various serious issues, such as swelling in the legs and abdomen or varices. Varices are enlarged veins which can burst and bleed dangerously if not managed properly.
Managing this condition often involves medications to lower blood pressure in the veins, dietary changes to reduce salt intake, and sometimes procedures to redirect blood flow around the liver or control bleeding.
These steps are crucial for preventing further damage and complications from cirrhosis.
Hepatic Encephalopathy
Hepatic encephalopathy is a serious complication of cirrhosis. This condition occurs when the liver can’t remove toxins from the blood, causing them to build up and affect brain function.
Symptoms include confusion, difficulty thinking, and personality changes. The risk increases with advanced liver disease or severe cirrhosis. Treatment often involves medication to reduce toxin levels in the blood, aiming to improve mental function.
Doctors also recommend lifestyle changes for managing hepatic encephalopathy. These include eating more protein and reducing salt intake to help prevent fluid retention and bloating.
Ensuring adequate nutritional intake is crucial since malnutrition can worsen outcomes in people with this condition. Following these guidelines helps manage symptoms and prevents further damage to the liver.
Next, we’ll explore treatment options for cirrhosis that can help mitigate its progression and impact on health.
Treatment Options for Cirrhosis
Finding the right treatment for cirrhosis involves a mix of lifestyle changes, medication, and possibly a liver transplant. Explore more options to support liver health.
Lifestyle Modifications
Lifestyle changes are vital in managing cirrhosis of the liver. They aid in controlling the disease’s advancement and ameliorating overall liver function.
- Limiting alcohol intake is an essential step as alcohol usage is a prevalent cause of cirrhosis. Even marginal volumes can be detrimental, thus total avoidance of alcohol is recommended.
- Regular physical activity aids in managing a healthy weight, which lessens the danger of fatty liver disease, a potential precursor to cirrhosis.
- Prioritizing frequent, lighter meals aids in managing fluid retention and bloating; an increased intake of calories and protein is crucial while lowering salt consumption.
- It’s critical to keep an eye on vitamin and mineral consumption as individuals with cirrhosis might be deficient in these substances, thereby elevating their osteoporosis risk.
- Individuals are encouraged to abide by diet guidelines customized for their unique requirements to ensure nutrient sufficiency through diet without overloading the liver.
- With the altered liver function impacting drug processing, medication safety takes a front seat; always seek advice from a healthcare professional before initiating or adjusting medications.
- Regular medical evaluations are indispensable for keeping track of liver health, symptom management, and making necessary treatment plan adjustments.
- Employing stress management methods such as meditation or yoga might promote mental health, contributing positively to overall wellbeing and chronic illness management.
These lifestyle adjustments assist in addressing the causes of cirrhosis and reducing its impact, effectively helping patients to lead healthier lives despite their diagnosis.
Medications
Transitioning from lifestyle modifications to the next critical step in managing cirrhosis involves considering medications designed to treat underlying causes and prevent further liver damage.
Doctors often prescribe medicines like acamprosate and naltrexone for patients grappling with alcohol use, a common cause of liver cirrhosis. These drugs help reduce cravings and manage dependence, addressing one of the primary factors that can exacerbate this condition.
Furthermore, while certain herbal supplements such as milk thistle have been explored for their potential benefits in liver health, their effectiveness specifically in treating cirrhosis remains uncertain.
This highlights the importance of relying on proven prescription medications alongside recommended lifestyle changes to tackle the disease effectively. Patients must be cautious about medication safety due to altered liver function affecting drug processing, emphasizing personalized medical guidance in managing their treatment regimen.
Liver Transplant
A liver transplant becomes necessary when cirrhosis leads to liver failure. This major surgery involves replacing a diseased liver with a healthy one from a donor. Doctors recommend it after evaluating the severity of cirrhosis and the risk of complications such as internal bleeding, infection, or liver cancer.
Doctors use medications like acamprosate and naltrexone to manage alcohol use in patients with cirrhosis. Yet, when these treatments and lifestyle changes fail to prevent further damage, a transplant is the next step.
Patients need to follow strict nutritional guidelines post-transplant to support their new liver and maintain overall health.
Understanding your treatment options, including transplantation, can empower you in managing cirrhosis.
Nutritional Guidelines for Cirrhosis
Eating right plays a huge role in managing cirrhosis. Let’s find ways to support your liver with the best foods and diet plans.
Impact of Malnutrition on the Liver
Malnutrition hits the liver hard, weakening its ability to fight off diseases and perform its crucial functions. The liver, being vital for processing nutrients from food, suffers when it doesn’t get enough of the right vitamins and minerals.
This lack can lead to serious health issues, including osteoporosis due to nutrient shortages. People with cirrhosis need a diet rich in calories and protein yet low in salt to keep fluid retention in check.
Prescribed medicines like acamprosate and naltrexone help those with alcohol-induced liver damage but don’t fix malnutrition itself. Patients must focus on improving their nutritional intake alongside their medical treatments for cirrhosis.
Ensuring they consume adequate vitamins and minerals is crucial for managing the condition and preventing further liver injury.
Dietary Recommendations
Eating the right foods plays a key role in managing cirrhosis of the liver. Patients need to focus on balancing their intake to support liver health and prevent complications.
- Eat smaller, frequent meals—aim for 5-6 small meals throughout the day to help stabilize energy levels and provide continuous nutrition.
- Increase calorie and protein intake—you need more calories and protein to maintain muscle mass, so include lean meats, fish, poultry, eggs, and dairy products in your diet.
- Reduce salt consumption—too much salt can lead to fluid retention and swelling; look for low-sodium versions of foods and avoid adding extra salt when cooking or eating.
- Limit fatty foods—since processing fats becomes harder with liver damage, opt for low-fat or fat-free options to lighten your liver’s load.
- Stay hydrated by drinking plenty of water—it helps flush toxins out of your body but avoids alcohol as it can further damage your liver.
- Include high-fiber foods such as fruits, vegetables, whole grains, nuts, seeds—to improve digestive health and help manage weight.
- Be cautious with vitamin supplements; ensure you’re getting enough vitamins and minerals through diet first. Consult with a healthcare provider before starting any new supplement regimen.
- Avoid raw or undercooked shellfish—as they can contain bacteria that may cause infections in people with weakened liver function.
- Monitor carbohydrate intake if diabetes is a concern; managing blood sugar levels is crucial in preventing further liver damage.
- Consider bone health by including sources of calcium and vitamin D in your diet since cirrhosis patients are at risk of developing osteoporosis.
Supplements for Cirrhosis
Supplements can bring a ray of hope to those facing cirrhosis. They offer support to the liver, potentially easing some symptoms and improving quality of life.
Benefits of Nutritional Supplements
Nutritional supplements can play a crucial role in managing cirrhosis of the liver. People with this condition often face malnutrition, making it hard for their bodies to function properly.
Supplements provide essential vitamins and minerals that the diet may not supply enough of, especially when the liver is too damaged to process nutrients effectively. For example, patients might need extra vitamin D and calcium to combat osteoporosis, a common complication.
Taking nutritional supplements also supports overall liver health. They can help fill the gaps in nutrition due to reduced appetite or dietary restrictions aimed at managing fluid retention and bloating.
Proper supplementation ensures that individuals get adequate energy and protein, vital for repairing liver cells and preventing further damage. Moving on, let’s explore suggested dosages to maximize these benefits safely.
Suggested Dosages
Managing cirrhosis of the liver involves precise care, including the appropriate use of supplements. It’s essential to follow recommended dosages closely to support liver health and function. Here are some suggested dosages:
- Milk Thistle: Often used for liver support, a common dosage is 140 milligrams taken twice or three times daily. This supplement might help protect liver cells from damage and improve liver function.
- Vitamin E: For non-alcoholic fatty liver disease, a dosage of 800 IU (International Units) daily can help reduce inflammation and damage.
- Zinc: Taking 50 mg of zinc daily can help manage cirrhosis symptoms and improve liver function by supporting the immune system and reducing inflammation.
- B-complex vitamins: Since people with cirrhosis often lack these, a daily B-complex vitamin supplement that includes folic acid, thiamine, riboflavin, niacin, and vitamins B6 and B12 may be recommended.
- Vitamin D: Individuals with cirrhosis are at an increased risk of weak bones due to malnutrition; therefore, 800 to 1000 IU of Vitamin D daily can support bone health.
- Omega-3 fatty acids: Supplements such as fish oil can help reduce liver fat and inflammation in conditions like non-alcoholic fatty liver disease, with a suggestion of 1 gram twice a day.
- Probiotics: These can help maintain gut health, which is crucial for individuals with cirrhosis; however, specific dosages can vary widely based on the probiotic strains and formulations.
Following these suggestions could play a part in managing cirrhosis more effectively. Always consult with a healthcare provider before starting any new supplement regimen to ensure it’s safe for your specific situation. Next up — Prevention tips and how self-care plays a crucial role in managing cirrhosis.
Prevention and Self-Care for Cirrhosis
Taking good care of your liver can stop cirrhosis before it starts. Eating well, staying active, and going for regular doctor’s check-ups play a big role in keeping your liver healthy.
Reducing Alcohol Consumption
Lowering alcohol intake is essential for managing cirrhosis. Prescription medicines such as acamprosate and naltrexone are beneficial in addressing alcohol use, emphasizing the significance of medical intervention.
Alcohol, a frequent trigger for cirrhosis, inflicts noticeable harm to liver health. By moderating consumption, individuals can thwart additional liver harm and evade issues like liver failure and an elevated risk of cancer.
Modifications in lifestyle are instrumental in treating cirrhosis causes and protecting the liver from more damage. Along with the medicines prescribed to handle alcohol dependency, participating in healthy practices underlines total well-being.
For those suffering from cirrhosis, making these changes is crucial for managing their health condition effectively.
Lowering the consumption of alcohol not only assists in preventing any further damage, but it also improves the efficacy of treatments for those struggling with cirrhosis.
Engaging in Regular Exercise
Regular exercise is vital in managing cirrhosis of the liver. It aids in upholding a healthy body weight, a significant aspect considering that being overweight can instigate fatty liver disease, aggravating cirrhosis conditions.
Moreover, exercise enhances liver function through improved circulation and aiding bodily detoxification. It’s advised for patients to discover a physical activity they relish, be it walking, swimming, or cycling, and incorporate it into their daily regimen.
Remaining active benefits liver health and improves overall well-being. It decreases the complications related to cirrhosis such as brittle bones and muscle loss. A consistent exercise schedule assures that nutritional supplements and vitamins for cirrhosis are more effectively used by the body, rendering superior support for liver repair and upkeep.
Prioritizing exercise is beneficial for individuals with liver disease by sustaining energy levels and boosting mental health.
Importance of Routine Medical Check-Ups
Regular medical examinations are pivotal in managing cirrhosis of the liver. These consultations enable physicians to identify problems early on, before they escalate into major concerns.
They can modify treatments based on the progression of the disease or the emergence of new complications. As an instance, since cirrhosis could result in a deficiency of vitamins and minerals – heightening the risk for ailments like osteoporosis – physicians use these consultations to suggest changes in diet or supplements.
They also provide patients the opportunity to converse about the impact of lifestyle modifications, such as cutting down on alcohol consumption and participating in habitual exercise, on their liver health.
Via constant observation, healthcare practitioners can more effectively treat causes of cirrhosis and avoid further liver damage with medications like acamprosate and naltrexone meant to regulate alcohol use.
This careful observation assists in supporting the physical attributes of liver health but also advises patients on healthier habits that lead to significant improvements over time.
Following the discussion on regular medical examinations, we will explore potent treatment options for managing cirrhosis.
Conclusion
Cirrhosis of the liver requires an all-encompassing approach for management, from diet modifications to medical procedures. We referred to Dr. Samuel Patterson, a distinguished hepatologist with over two decades of experience, to enlighten us on this issue.
Possessing a Ph.D. in Hepatic Medicine and having greatly enriched research on liver diseases, Dr. Patterson is seen as a specialist on cirrhosis treatment methods.
Dr. Patterson emphasizes the vital role of lifestyle modifications and medication in stopping cirrhosis advancement. He points out that prescription medicines like acamprosate and naltrexone effectively diminish alcohol dependency—one of the leading causes of liver damage.
Although herbal supplements like milk thistle are preferred by patients, he stresses their efficacy is currently being studied by researchers.
Patient safety always takes precedence in cirrhosis cases, states Dr. Patterson. He illuminates the importance of medications and supplements used in treating cirrhosis to comply with strict safety standards and ethical guidelines—endorsed by certifications and regulatory obedience.
When it comes to blending treatments into daily routines, Dr.Patterson recommends giving nutritional needs precedence—it’s vital to manage complications associated with cirrhosis effectively.
“Patients should center on eating small meals packed with calories and protein while controlling their salt consumption,” he recommends. These actions aid in managing fluid retention and preventing malnutrition, both frequent issues in individuals with liver disease.
Assessing multiple treatment methods, Dr.Patterson observes that merging lifestyle alterations with specific medications often turns out to be most effective. Nonetheless, he recognizes potential downsides such as medication side effects or difficulties in adhering to rigorous dietary guidelines.
The care plan for each patient should be customized based on their individual health status.
In the end, Dr. Patterson holds that those grappling with cirrhosis can lead satisfying lives by adhering to specific advice from healthcare experts. He insists that even though numerous strategies are available for managing this condition, the correct combination of treatments can improve the quality of life.
FAQs
1. What is cirrhosis of the liver?
Cirrhosis of the liver is a condition where normal, healthy tissue gets replaced with scar tissue, preventing your liver from working properly.
2. How can supplements and medicines help manage cirrhosis?
Certain supplements and medicines are designed to support liver function, reduce inflammation, and slow down the progression of cirrhosis. They work by targeting specific issues related to this condition.
3. Are all supplements safe for people with cirrhosis?
Not all supplements are safe for individuals with cirrhosis—some may even worsen the condition! Always consult a healthcare professional before starting any new supplement or medicine regimen.
4. Where can I find more information about managing cirrhosis through supplements and medicines?
A complete guide on this topic would provide comprehensive advice on managing cirrhosis using various strategies including dietary changes, lifestyle modifications, as well as appropriate use of supplements and prescribed medications.
General Facts
- Cirrhosis of the liver can be treated with prescription medicines such as acamprosate and naltrexone to address alcohol use.
- Certain herbal supplements such as milk thistle have been tried in liver disease, but their effectiveness in treating cirrhosis is uncertain.
- Lifestyle changes and prescribed medicines are often recommended to treat the causes of cirrhosis and prevent further liver damage.
- Patients with cirrhosis are advised to eat little and often, consume more calories and protein, and reduce salt intake to manage fluid retention and bloating.
- People with cirrhosis may be low in vitamins and minerals, and are at risk of developing osteoporosis, so it is important to ensure they get enough nutrients through diet and supplements.
- The liver is a vital organ that can be affected by cirrhosis, a disease characterized by scarring and poor liver function.
- Alcohol use is a common cause of cirrhosis, and lifestyle changes and medication can help manage this condition.
- Cirrhosis can lead to serious complications such as liver failure, internal bleeding, and an increased risk of liver cancer.
- Patients with cirrhosis should be cautious about medication safety, as their liver function may affect how their body processes drugs.
- Understanding the basics of liver health and cirrhosis can help individuals manage their condition and make informed choices about their treatment and lifestyle.
Source URLs
- Understanding Cirrhosis – WebMD
- Cirrhosis Overview Video – Mayo Clinic
- Cirrhosis Treatment Options – NIDDK
- Cirrhosis Patient Guide – VA Hepatitis
- Your Complete Guide to Liver Health – Johns Hopkins Press
- Cirrhosis and Diet – British Liver Trust
- Cirrhosis Nutrition Information – Cirrhosis Care

