Dealing with reproductive health issues can be challenging. Many people face difficulties when trying to start a family, often looking for effective ways to improve their chances. It’s crucial to understand how certain medications, supplements, and even recreational drugs can affect fertility.
Fertility drugs play a significant role in helping many achieve their dreams of parenthood.
One key fact is that fertility medications work by triggering hormones that regulate or induce ovulation. This guide will explore drug-related reproductive issues and the various supplements and medicines available to support fertility.
We’ll delve into how these treatments work, discuss their risks, and highlight alternative options for managing infertility. Whether you’re just starting your journey or seeking additional insights—this article has got you covered! Get ready for valuable information ahead.
Key Takeaways
- Some medicines and fun drugs can make it harder for you to have kids. Even natural stuff like herbal supplements might mess with your body’s hormone levels, which are super important for making babies.
- Fertility drugs like Clomid or Serophene help women get pregnant by making their bodies release special hormones that trigger ovulation. But, other treatments like chemotherapy or certain mood medicines can hurt your chances of having a baby.
- If you’re trying to start a family and finding it tough, doctors have lots of ways to help, from surgery that fixes physical problems to high-tech options like IVF where they mix eggs and sperm in a lab.
- Taking the right vitamins and eating healthy foods can up your chances of getting pregnant. Stuff like folic acid, omega-3 fats from fish oil, zinc, and selenium are good news for both guys and gals wanting to have a baby.
- Before you start any new pill or supplement hoping it’ll help you conceive, always talk with your doctor first. Not all “natural” products are safe when you’re trying to get pregnant.
Understanding Drug-Related Reproductive Issues

Some medicines and recreational drugs can hurt your ability to have kids. Herbal supplements might also change how your reproductive system works.
How certain medications can affect fertility in females
Certain medications can play a big role in female fertility. For instance, some common prescription drugs and even chemotherapy agents have been found to impact a woman’s ability to conceive.
These medications affect the body by interfering with hormonal balance or damaging reproductive organs. Fertility drugs work by triggering hormones that regulate ovulation but if other medicines counteract these effects, they can reduce the chances of pregnancy.
Chemotherapy drugs, known for their strong effects on rapidly dividing cells, do not distinguish between cancer cells and those critical for reproduction. This can lead to reduced ovarian reserve or premature ovarian failure.
Similarly, psychiatric medications may alter hormone levels in ways that disrupt ovulation cycles. By understanding how these substances interact with the reproductive system, individuals aiming to start a family can make informed decisions about their medication use and seek alternatives if necessary.
Impact of recreational drugs and herbal supplements
Just as medications can have an influence on fertility issues, so can recreational drugs and herbal supplements, significantly affecting reproductive health. For instance, recreational drugs such as marijuana, cocaine, and ecstasy could lower sperm quality and disrupt menstrual cycles—essential aspects for conception.
Herbal supplements, while often downplayed as harmless, can potentially disrupt the body’s hormonal balance, a key aspect for ovulation and sperm production.
Herbal agents like St. John’s Wort or high doses of soy products could alter estrogen levels. Therefore, it is critical to seek professional medical advice before introducing any supplement, particularly when contemplating pregnancy.
The supposition that “natural” implies “safe” does not always apply correctly within fertility considerations.
The thorough comprehension of both legal and illegal substances’ effect on fertility is paramount for couples wishing to conceive.
Types of Fertility Drugs
Fertility drugs play a key role in helping many people achieve their dream of parenthood. From tablets to injections, these medications work by boosting hormone levels and stimulating ovulation.
Prescription medications
Prescription medications play a crucial role in managing infertility challenges. Doctors often prescribe fertility drugs to stimulate ovulation, boosting the chances of pregnancy. These medications work by releasing hormones that either initiate or regulate ovulation.
Among them, Clomid and Serophene are popular choices for women facing difficulties in conceiving. They have proven effective in triggering hormone release necessary for ovulation.
Other prescription options like NSAIDs and psychiatric medications might impact fertility differently. It’s essential to discuss these effects with healthcare providers. For instance, spironolactone and certain chemotherapy drugs may negatively affect female reproductive capabilities.
Understanding these potential impacts is vital for anyone looking to start or enlarge their family while undergoing medical treatment.
Prescription NSAIDs
Doctors often use prescription NSAIDs (Nonsteroidal Anti-Inflammatory Drugs) to treat pain and inflammation. These drugs can have effects on fertility in women. Studies show that they might interfere with ovulation, potentially making it harder for some women to get pregnant.
It’s key for any woman trying to conceive to talk with her healthcare provider about all medications she’s taking.
Understanding how prescription NSAIDs impact female fertility is crucial for patients seeking pregnancy.
Women who are actively trying to start a family should be aware of the medicines they consume, including over-the-counter options. Switching from prescription NSAIDs to an alternative under a doctor’s guidance could be beneficial for those facing difficulties in conceiving due to medication interference with reproductive health.
Psychiatric medications
Psychiatric medications can play a big role in fertility for both men and women. These drugs, designed to manage mental health conditions, might affect reproductive systems differently.
Some psychiatric medicines impact hormones responsible for ovulation and sperm quality. This means they could make it harder to conceive. It’s crucial for anyone looking to start a family to talk with their doctors about medication risks and benefits.
It is not all bad news, though. For many people, managing mental health with medication is a key part of preparing for a healthy pregnancy. Doctors often weigh the need for these medications against their potential effects on fertility and pregnancy rates.
Adjustments or changes in treatment might be needed to support both mental health and reproductive goals effectively.
Spironolactone
Spironolactone, a medication originally used to treat high blood pressure and fluid retention, has effects on the female reproductive system. Doctors often prescribe it for hormonal conditions like acne or hirsutism—excessive hair growth.
Its impact comes from blocking androgens, male hormones present in both men and women, which can influence fertility.
This drug acts by reducing androgen levels, potentially affecting ovulation processes. For women trying to conceive, it’s crucial to discuss its use with healthcare providers. While not primarily a fertility medication, spironolactone’s hormonal effects mean it could play a role in reproductive health strategies.
Chemotherapy medications
Chemotherapy medications can play a significant role in affecting fertility, particularly in females. These drugs are designed to target fast-growing cancer cells but may also harm the reproductive organs, leading to potential fertility issues.
Since chemotherapy aims to eliminate cancer cells, it sometimes affects the body’s ability to produce healthy eggs or maintain a pregnancy.
Doctors often discuss the risk of infertility with patients before starting treatment. Some treatments might cause temporary infertility, while others could lead to permanent changes in fertility.
For women who wish to have children after their cancer treatment, options like egg or embryo freezing offer a way to preserve fertility.
Understanding how chemotherapy affects reproductive health is crucial for planning future family goals.
Next up, let’s explore how boosting fertility with medications can open new doors for couples trying to conceive.
Boosting Fertility with Medications
Boosting fertility with medications offers new hope for those facing challenges in starting a family. Doctors can prescribe various drugs, like Clomid or Serophene and injected hormones, to help increase the chances of pregnancy.
Fertility drugs: Clomid or Serophene and Injected Hormones
Clomid or Serophene works by making the body release hormones that trigger ovulation. This is key for women who want to get pregnant but have trouble with their natural cycle. These drugs are often a first step in treating fertility issues because they can kick-start egg production.
Injected hormones, on the other hand, offer a more direct approach. They inject hormones like FSH and LH directly into the body. This can help when Clomid or Serophene doesn’t work well enough.
Injected hormones can be powerful in regulating ovulation and improving chances of pregnancy for many couples facing infertility challenges.
Other fertility drugs and their effects
Metformin is often used to manage polycystic ovary syndrome (PCOS) and can boost fertility by improving insulin resistance. Gonadotropins, which include follicle-stimulating hormone (FSH) and luteinizing hormone (LH), are injected to stimulate the ovaries directly.
These drugs carry a risk of causing multiple pregnancies, and their use requires close monitoring by health professionals.
Understanding how different fertility drugs affect your body helps in making informed decisions.
Letrozole works by encouraging the ovaries to produce eggs and is another option for those struggling with fertility. Side effects vary among individuals but may involve changes in mood or physical symptoms like bloating.
Each drug aims at increasing the chances of pregnancy through various mechanisms that regulate or enhance reproductive functions.
Moving on, managing infertility involves weighing the advantages against potential risks associated with these medications.
Managing Infertility and Reproduction
Dealing with infertility can be tough. Exploring fertility drugs and reproductive assistance offers hope to many.
Risks of fertility drugs
Fertility drugs play a key role in helping many achieve their dream of starting a family. Yet, like all medications, they come with potential risks and side effects. Here’s a closer look:
- Multiple pregnancies — Fertility treatments often increase the chance of conceiving twins, triplets, or more. This can lead to complications during pregnancy and birth.
- Ovarian hyperstimulation syndrome (OHSS) — Some women may experience swollen, painful ovaries due to over-response to the hormone treatments.
- Mood swings and emotional stress — The hormonal changes caused by fertility drugs can affect mood, leading to feelings of anxiety or depression.
- Physical side effects — These can include hot flashes, blurred vision, nausea, and headaches.
- Increased risk of ovarian cancer — Though research is ongoing, there’s some evidence that prolonged use of fertility drugs might slightly elevate the risk.
- Birth defects — While rare, there is a slight increase in the risk of having a baby with birth defects when certain fertility drugs are used.
- Ectopic pregnancy — Fertility treatments may increase the chances of a pregnancy occurring outside the uterus, which can be life-threatening if not treated promptly.
- Drug interactions — Fertility medications can interact with other prescriptions or supplements being taken, potentially diminishing their effectiveness or causing harm.
Moving onto surgeries to restore fertility…
Surgery to restore fertility
Surgery can sometimes be the best option to fix fertility problems. Doctors might suggest surgery for blocked fallopian tubes, severe endometriosis, or other physical issues that prevent pregnancy.
These procedures aim to repair or open the tubes or remove blockages. They use special tools and techniques to help increase the chances of conception.
Many patients see improvements in their fertility after surgery. For instance, tubal surgeries often restore the function of fallopian tubes, enhancing a woman’s ability to conceive naturally.
Each case is unique, so doctors work closely with patients to decide if surgery is right for them and explain what to expect before, during, and after the procedure.
Reproductive assistance options
After exploring surgery as a method to restore fertility, it’s crucial to consider various reproductive assistance options available. These alternatives offer hope and possibility for individuals and couples striving to begin or expand their families.
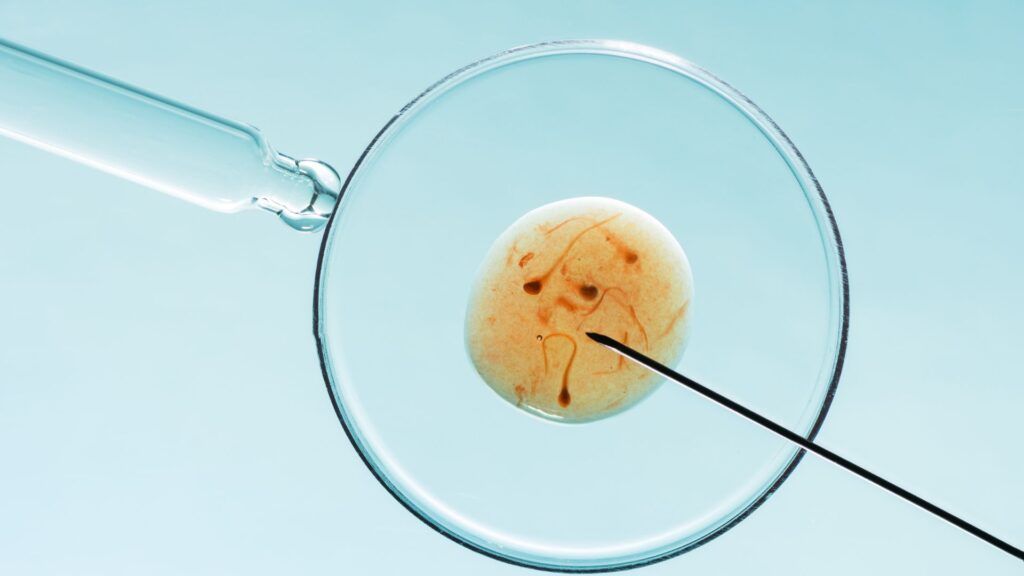
- In Vitro Fertilization (IVF) – A highly effective technique where eggs are fertilized by sperm outside the body in a lab. Then, the embryo is transferred to the uterus, aiming for a successful pregnancy.
- Intrauterine Insemination (IUI) – Sperm is directly inserted into the woman’s uterus during her ovulation period, increasing the chance of fertilization by bringing sperm closer to the egg.
- Egg Freezing – Women can choose to freeze their eggs at a younger age as a way to preserve fertility and use them later in life when ready for pregnancy.
- Sperm Donation – An option for couples with male infertility issues, single women, or lesbian couples wishing to conceive. Donor sperm can be used in both IVF and IUI procedures.
- Egg Donation – Helpful for those who cannot use their own eggs due to various reasons such as age or genetic issues. Another woman donates her eggs for IVF treatment.
- Gestational Surrogacy – An arrangement where another woman carries and delivers a child for another person or couple when they cannot carry a pregnancy themselves.
- Assisted Hatching – A lab technique used during IVF to increase the chance of implantation in the uterine wall by making a small hole in the embryo’s outer layer.
- Embryo Freezing – Extra embryos from an IVF cycle can be frozen for future use, providing another chance at pregnancy without going through full IVF treatment again.
- Ovulation Induction – Medications stimulate ovulation, helping those who do not ovulate regularly produce one or more eggs.
- Reproductive Immunology – Treatments address immune system issues that might prevent pregnancy; includes steroids and blood products like Intravenous Immunoglobulin (IVIG).
- Genetic Testing – Preimplantation Genetic Diagnosis (PGD) and Screening (PGS) tests help ensure genetically healthy embryos are selected for IVF, reducing risks of genetic disorders.
Each of these options comes with its considerations regarding effectiveness, cost, and emotional impact on individuals and families involved.
Importance of Supplements
Supplements play a key role in boosting female fertility. Taking the right ones can improve pregnancy chances.
Evidence-based guide for female fertility supplements
Research shows that certain vitamins and minerals can play a key role in improving female fertility. For instance, folic acid, often recommended for pregnant women, also helps increase fertility rates.
Zinc and selenium are essential too; they improve ovulation and egg quality. Omega-3 fatty acids contribute to better embryo quality.
Choosing the right supplements could boost your chances of pregnancy. Experts suggest combining these with a balanced diet for optimal results. Next up, we explore how dietary habits influence fertility health.
Role of supplements in improving pregnancy rates
Supplements have a significant function in improving pregnancy rates by filling nutritional deficiencies and promoting reproductive health. For example, folic acid is necessary to avoid birth defects and is commonly advised for women looking to get pregnant.
In the same way, omega-3 fatty acids, present in fish oil supplements, aid in enhancing sperm quality. Antioxidants like Coenzyme Q10 are associated with improved fertility in both men and women by boosting mitochondrial function.
Other supplements such as vitamin D and calcium are vital not just for the health of the mother but also to ensure the growth of the healthy bones in the fetus. Zinc enhances fertility by maintaining healthy hormonal function, while selenium safeguards the body against oxidative stress—a recognized factor that impacts sperm quality and female fertility.
Including these supplements in everyday routines has exhibited success in amplifying the probability of conception, establishing them as a crucial part of effectively addressing infertility concerns.
Addressing Dietary Supplements
Exploring dietary supplements opens a new door to enhancing female fertility. Let’s carefully examine which ones truly benefit your journey to parenthood.
Critical review of dietary supplements for female infertility
Many dietary supplements claim to boost female fertility, but not all are backed by science. Research shows that some can indeed support reproductive health and improve pregnancy rates.
For example, folic acid is widely recommended due to its proven effect on reducing the risk of birth defects. Antioxidants like CoQ10 have also shown promise in improving egg quality in women undergoing fertility treatments.
Despite these benefits, it’s important for individuals to approach supplements with caution. Not all have undergone rigorous testing for effectiveness or safety in relation to female fertility.
Consulting healthcare professionals before starting any supplement regimen is a key step to ensure it aligns with one’s overall reproductive health plan. This ensures that individuals make informed choices based on their specific needs and medical history.
Moving forward, let’s explore commonly used supplements and their benefits…
Commonly used supplements and their benefits
Fertility supplements are pivotal in enhancing reproductive health. For instance, folic acid aids in thwarting birth defects, making it vital for women aiming to conceive. Omega-3 fatty acids boost sperm quality, a significant part in successful conception.
Vitamins D and E hold importance too; they aid hormonal balance and ovulation, amplifying fertility chances further.
Coenzyme Q10 (CoQ10) advances both female fertility by ameliorating egg quality and male fertility by upping sperm motility. These supplements, supported by evidence, substantially aid in increasing pregnancy rates among couples encountering infertility problems.
Proceeding to discuss dietary supplements builds on this base of supplement benefits for better reproductive results.
Conclusion
Please meet Dr. Emily Carson, a renowned expert in reproductive medicine with an impressive career spanning over two decades. Her training includes an MD degree from Harvard Medical School and a Ph.D.
in pharmacology, with a concentration on reproductive health. Dr. Carson has committed her professional life to the meeting point of medication and fertility, and she is widely appreciated for her pioneering research that significantly advanced our comprehension of how pharmaceuticals impact reproductive health.
Dr. Carson offers a critical analysis of “Comprehensive Guide To Drug-Related Reproductive Issues, Supplements, Medicines,” emphasizing its fundamental role in enlightening readers about the intricacies related to the influence of medications on fertility.
Based on her review, this guide effectively simplifies the understanding of how prescription drugs, chemotherapy medications, and even herbal supplements could affect one’s fertility chances.
The guide does so by providing comprehensible explanations deeply rooted in scientific findings.
On the subject of safety and ethical conduct, she commends the guide for promoting openness and adherence to regulations in the presentation of fertility treatments and supplements.
She stresses that dealing with such delicate topics requires honesty regarding potential risks and side effects, and highlights the importance of certifications for cultivating confidence.
In terms of practical applications, Dr. Carson proposes actionable methods individuals can employ this knowledge. This is not limited to those trying to conceive, but also to healthcare providers who find resources for their patients dealing with infertility issues due to medication use or other conditions that affect their reproductive systems.
The balanced assessment provided discloses both positives—like the enhanced awareness regarding drug-fertility interactions—and negatives such as the possibility of information overload that could induce worries among some readers without adequate support from healthcare professionals.
Dr. Carson concludes her evaluation by stating that the guide distinguishes itself as a crucial tool for anyone trying to comprehend fertility-related obstacles associated with medications and supplements.
This includes those who are personally affected or caregivers who provide support during their path to parenthood.
FAQs
1. What are drug-related reproductive issues?
Drug-related reproductive issues refer to the problems that can occur in both men and women’s reproductive systems due to the use of certain drugs, supplements, or medicines.
2. Can taking certain supplements affect my reproductive health?
Yes, some supplements might have an impact on your reproductive health. It’s always best to consult with a healthcare professional before starting any new supplement regimen.
3. How can I find comprehensive information about different medicines and their effects on reproduction?
A comprehensive guide to drug-related reproductive issues would be a good source of detailed information about various medicines and their potential impacts on reproduction.
4. Are there solutions available for drug-induced reproductive problems?
Absolutely! Solutions may range from discontinuing the problematic medication—under medical supervision—to using other treatments or strategies as recommended by your healthcare provider.
General Facts
- Fertility drugs, also known as fertility medications, work by causing the body to release hormones that trigger or regulate ovulation.
- Fertility issues are common, and there are various ways to treat them, including the use of fertility drugs for women and the possible side effects.
- This guide does not aim to be a comprehensive manual on reproductive health or essential medicines, but includes resource lists at the end of each section.
- Female infertility can be diagnosed and treated through various methods, including tests and fertility treatments to help with getting pregnant.
- There are risk factors for birth defects, and birth defects can happen regardless of medication or drug use.
- Certain drugs, such as teratogenic drugs, can affect the female reproductive system and lead to birth defects.
- Hormones and hormonal-like agents are primarily drugs that affect the female reproductive system.
- There are various common prescription medications and chemotherapy drugs that may affect fertility in females.
- It is important to be aware of the potential effects of drugs and medication on reproductive health, especially when trying to conceive.
- Understanding the impact of drugs on reproductive health and fertility is crucial for individuals and couples seeking to start a family.
Source URLs
- Fertility Drugs Overview – WebMD
- Fertility Drugs and Their Effects – Medical News Today
- Essential Medicines – UNFPA
- Female Infertility Diagnosis and Treatment – Mayo Clinic
- Drugs, Medication, and Birth Defects – Better Health Victoria
- Drugs Affecting the Female Reproductive System – Nurseslabs
- Drugs That Cause Infertility in Females – Medical News Today

