Talking about vaginal cancer can feel scary, but knowing what to watch for and how it’s treated is a big step toward taking charge of your health. Many people don’t know the symptoms or options available if they’re diagnosed.
One key fact? Vaginal cancer is rare, affecting women mostly over the age of 50, yet awareness and early detection can significantly improve outcomes.
This blog walks you through everything from spotting the warning signs to understanding your treatment choices—including surgery, chemotherapy, and more. We’ll also explore how supplements and medicines play into recovery and well-being.
Ready to learn more? Keep reading.
Key Takeaways
- Vaginal cancer is a rare disease mostly affecting women over 50, but catching it early can save lives. Pay attention to symptoms like abnormal bleeding and pain during intercourse.
- Treatment for vaginal cancer varies from surgery and radiation therapy to chemotherapy and targeted therapies. Each treatment aims at eliminating cancer while maintaining quality of life.
- Regular pelvic exams, Pap tests, and getting the HPV vaccine are essential steps in preventing vaginal cancer. These measures help detect changes early or prevent them altogether.
- Supplements and a healthy diet can support treatment by boosting the immune system. However, always consult with a doctor before adding any new supplements to avoid interactions with treatments.
- Support services exist for those dealing with vaginal cancer, offering emotional, nutritional, and financial assistance to patients and their families throughout their journey.
Understanding Vaginal Cancer

Vaginal cancer is a rare disease that starts in the vagina. Learning about its types and risk factors can help women take early action.
Types of Vaginal Cancer
There are two main types of vaginal cancer that doctors typically diagnose. The first type, squamous cell carcinoma, starts in the thin, flat cells lining the vagina and is found in 85% of cases.
It usually grows slowly and often begins on the upper part of the vagina. The second type is adenocarcinoma, which begins in the glandular cells that line the walls of the vagina. This form can spread more quickly than squamous cell carcinoma.
Understanding these differences helps doctors create effective treatment plans. After identifying the type, they look into what causes vaginal cancer and its risk factors to tailor their approach further.
Causes and Risk Factors
Several factors raise the risk of developing vaginal cancer, a rare condition where malignant cells form in the vagina. Age stands out as a primary concern—vaginal cancer most often hits women over 50 years old.
Smoking adds to the danger, with its harmful effects reaching far beyond just lung health. A history of cervical cancer or an infection with human papillomavirus (HPV) significantly increases this risk, pointing toward the virus’s role in various cancers.
Understanding why some develop this disease while others don’t hinges on recognizing these risks. HPV vaccination emerges as a powerful preventive measure, especially notable for its ability to fend off types of HPV linked to vaginal and other gynecological cancers.
Regular pelvic exams and Pap tests are crucial strategies for early detection, making it easier to catch signs before they escalate into more serious conditions.
Symptoms to Look Out For
Vaginal cancer symptoms can be easy to miss. It’s crucial to pay attention to your body and notice any changes.
- Abnormal vaginal bleeding, especially after intercourse, could be a serious sign.
- Unusual vaginal discharge that might have a foul smell or be tinged with blood needs attention.
- Pain during intercourse often indicates something isn’t right.
- A noticeable lump or mass in the vagina that you can feel suggests the need for a professional check-up.
- Frequent urination or feeling the need to urinate without much result could signal an issue.
- Pelvic pain, not related to your menstrual cycle or other known conditions, may be concerning.
- Constipation or changes in bowel habits can also indicate vaginal cancer among other possibilities.
- Itching or irritation inside the vagina or on the vulva should not be ignored.
- Swelling of the legs can occur if cancer affects lymphatic drainage.
Knowing these symptoms helps in early detection and treatment of vaginal cancer.
Diagnosis and Staging
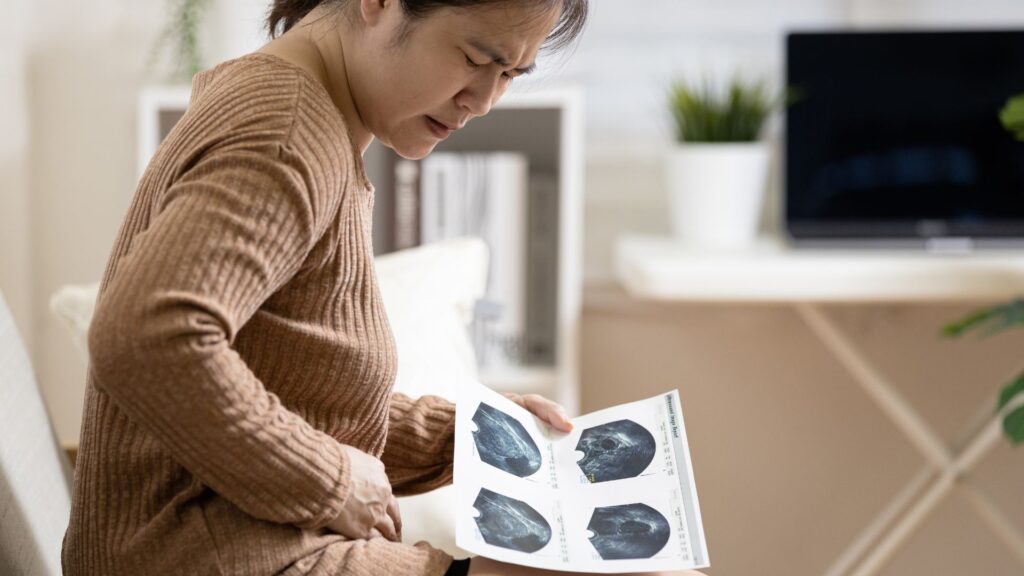
Doctors use several tests to diagnose vaginal cancer. They start with a pelvic exam to feel for any lumps or irregularities. A Pap test may follow, where cells are collected from the vagina and examined for abnormalities.
If these tests suggest cancer, a biopsy is conducted. Here, a small piece of tissue is removed and studied under a microscope to confirm the presence of cancer cells.
Imaging tests like MRI or CT scans help determine the cancer’s stage—how far it has spread within the vagina or to other parts of the body. Staging is crucial because it guides treatment decisions and helps predict outcomes.
Treatment Options
Exploring treatment options for vaginal cancer offers multiple paths, including surgery and chemotherapy—each customized to patient needs. Keep reading to discover how these treatments work and what might be best for you.
Surgery
Doctors often choose surgery as a key treatment for vaginal cancer. They aim to remove cancer cells while preserving the vagina’s function as much as possible. Types of surgery vary based on the cancer’s size and stage.
For early-stage cancers, a surgeon might only need to remove a small part of the vagina. With more advanced cases, more extensive procedures are necessary, sometimes including removal of surrounding tissues or organs.
In certain situations, reconstructive surgery can help restore appearance and function after major operations. Surgeons work closely with patients to decide the best approach, considering factors like the cancer’s spread and overall health.
Each surgical option comes with different risks and recovery times, which doctors discuss beforehand to prepare patients for what lies ahead.
Radiation Therapy
Moving on from surgery as a treatment option, radiation therapy presents another vital path in battling vaginal cancer. This method uses high-energy rays to target and destroy cancer cells, carefully focusing on affected areas while sparing surrounding healthy tissue.
Experts carefully plan each session to maximize the impact on malignant cells and minimize harm to the rest of the body.
Radiation therapy can be external, where machines send radiation toward the cancer from outside the body, or internal—known as brachytherapy—where radioactive materials are placed inside the vagina near the cancer cells.
Both methods have shown effectiveness in treating vaginal cancer, either used alone or combined with other treatments like chemotherapy for enhanced results. Patients may experience side effects such as fatigue or skin irritation around the treated area; these are typically temporary and manageable under medical guidance.
Radiation therapy remains a cornerstone in eradicating vaginal cancer cells while preserving patient quality of life.
Chemotherapy
After exploring radiation therapy as a vital treatment method for vaginal cancer, chemotherapy emerges as another critical option. This approach uses powerful drugs to kill cancer cells throughout the body.
Doctors often recommend chemotherapy when vaginal cancer has spread beyond the vagina or to decrease the risk of return.
Chemotherapy can be given in different ways—through an IV directly into a vein, as pills you swallow, or sometimes both. The choice depends on the type and stage of cancer you’re facing.
Side effects might include fatigue, hair loss, and nausea but vary widely from person to person. Fortunately, there are treatments and strategies to manage these side effects effectively.
Targeted Therapy
Moving on from chemotherapy, targeted therapy presents a more focused approach to combat vaginal cancer. This treatment zeroes in on specific genes, proteins, or the tissue environment that contributes to cancer’s growth and survival.
Unlike chemotherapy that affects all rapidly dividing cells, targeted therapies aim at the cancer’s specific characteristics.
Doctors use these drugs to block the growth and spread of cancer cells while minimizing damage to healthy ones. Medications like hormone therapy target cancer’s specific hormones it needs to grow.
Targeted treatments offer a beacon of hope for patients with advanced vaginal cancer, providing options when traditional methods may fall short.
Alternative or Complementary Treatments
Many people with vaginal cancer explore treatments beyond surgery, chemotherapy, and radiation. They might use these methods to ease side effects or boost well-being. Options like acupuncture help manage pain and reduce nausea after chemo.
Yoga and meditation are great for stress relief. Some also try herbal supplements, but it’s vital to talk with a doctor first—they can clash with cancer drugs.
Diet changes can make a difference too. Eating plenty of fruits, vegetables, and whole grains supports overall health during treatment. Doctors often suggest consulting a nutritionist who specializes in cancer care.
These alternative approaches are not cures but they offer comfort and control over one’s healing journey.
Palliative Care
Palliative care focuses on improving the quality of life for patients dealing with serious illnesses like vaginal cancer. It aims to ease symptoms and relieve pain, addressing not just physical needs but emotional and spiritual ones too.
Teams of healthcare professionals work together to support both the patient and their families through this tough journey.
Palliative care is about caring, not curing, but making every day count.
This type of care can start at any point during treatment, helping manage side effects from treatments such as chemotherapy or radiation therapy. The goal is simple – make each day more comfortable for those facing the challenges of vaginal cancer.
Supplements and Medicines to Support Treatment
Choosing the right supplements and medicines can make a huge difference in treating vaginal cancer. They help your body stay strong and may lessen side effects of other treatments.
Importance of Nutrition and Supplements
Eating healthy foods and taking the right supplements can make a big difference in how your body fights vaginal cancer. Different vitamins, minerals, and nutrients give your immune system a boost.
They help your cells grow properly and can even make treatments work better. For example, some studies suggest that vitamin D might play a role in stopping or slowing down cancer growth.
Always talk to your doctor first about which supplements are safe for you.
Certain medicines used in treating vaginal cancer, like chemotherapy drugs, can be very tough on your body. This is where nutrition comes into play – it’s key to recovery and strength during treatment.
Foods rich in antioxidants—like fruits, vegetables, nuts, and seeds—can protect your cells from damage. Moreover, protein keeps muscles strong, important when fighting cancer or recovering from surgery.
Combining good nutrition with the right supplements under a doctor’s guidance ensures you’re supporting your body as much as possible through treatment.
Commonly Used Medicines
After discussing the importance of nutrition and supplements, it’s crucial to highlight the medicines commonly used in treating vaginal cancer. These medications are designed to fight cancer cells and manage symptoms.
- Chemotherapy drugs, like Cisplatin and Carboplatin, attack fast-growing cancer cells throughout the body.
- Hormone therapy medicines, such as Progestin, help slow the growth of certain types of vaginal cancer cells that respond to hormones.
- Targeted therapy drugs focus on specific weaknesses present within cancer cells, blocking their growth and spread. For example, Bevacizumab targets a protein that helps tumors grow blood vessels.
- Immunotherapy treatments boost the body’s natural defenses to fight the cancer. Pembrolizumab is a type of immunotherapy used in some cases.
- Pain relievers and anti-inflammatory drugs alleviate discomfort and improve quality of life during treatment.
- Anti-nausea medications prevent or reduce nausea caused by chemotherapy and radiation therapy.
- Antibiotics treat infections that may occur during treatment as the immune system becomes compromised.
- Bone health agents, like Bisphosphonates, help manage bone loss associated with cancer treatment.
Understanding these medications can empower patients as they work through their treatment journey with their healthcare team.
Coping and Support
Living with vaginal cancer brings challenges, but support is out there. Many resources and programs can help you manage your journey.
Living with Vaginal Cancer
Living with vaginal cancer can be challenging. Patients often face physical and emotional struggles. They might deal with symptoms like pain or discomfort, which affect daily life.
Many seek support from friends, family, or support groups to share their experiences and coping strategies. Doctors also recommend counseling to help manage feelings of anxiety or sadness.
Patients are encouraged to stay active and eat a healthy diet to strengthen their bodies against the effects of treatment such as chemotherapy or radiation therapy. Regular check-ups are crucial for monitoring health and adjusting treatments if needed.
Staying informed about the condition helps patients make educated decisions about their care.
Patient Resources and Programs
Dealing with vaginal cancer presents unique challenges for patients and their families. Support is available through various patient resources and programs designed to help at every step of the journey.
- Cancer Support Communities offer emotional support and education for patients, caregivers, and family members. These communities can be found in many towns and cities, providing a safe space to share experiences and advice.
- Financial Assistance Programs help ease the burden of treatment costs. Many organizations offer grants, loans, or guidance on managing medical expenses.
- Nutritional Counseling Services are vital for maintaining strength during treatment. Dietitians specializing in cancer care can create personalized eating plans that support healing and recovery.
- Rehabilitation Services focus on improving quality of life through physical therapy, occupational therapy, and speech therapy if needed. These services aim to help patients regain independence post-treatment.
- Cancer Hotlines and Information Centers provide answers to medical questions, information on the latest treatments, and guidance on living with cancer. They are staffed by knowledgeable healthcare professionals.
- Online Support Forums allow patients to connect with others facing similar challenges from the comfort of their home. These platforms offer anonymity and 24/7 accessibility.
- Legal Aid Services assist patients facing discrimination due to their diagnosis or needing help with insurance claims and other legal matters related to their illness.
- Transportation Services help patients get to and from appointments when they cannot drive themselves or do not have access to public transportation.
- Home Health Care Services support patients who require professional medical care at home during recovery stages or for palliative care needs.
- Educational Workshops, both online and in-person, cover topics relevant to cancer care, including understanding treatments, side effects management, and wellness strategies.
- .Mouse over each item for more detailed information about how these resources can provide critical support throughout the treatment process.
Prevention and Early Detection
Preventing vaginal cancer starts with regular checks. Get your pelvic exams and HPV vaccines to catch problems early.
Regular Pelvic Exams and Pap Tests
Regular pelvic exams and Pap tests are key steps in preventing vaginal cancer. These exams help find any changes in the vagina early, when the chance of treatment being successful is higher.
- What happens during a pelvic exam? A healthcare provider checks the vagina, cervix, fallopian tubes, vulva, ovaries, and uterus for any abnormalities.
- The Pap test process involves collecting cells from the cervix with a small brush or spatula to check for precancerous or cancerous cells.
- How often should you get these exams? Women should start having pelvic exams at age 21 and continue every three years if their Pap test results are normal.
- Importance of HPV testing: Alongside a Pap test, an HPV test checks for the virus that can cause cell changes on the cervix.
- Follow-up after abnormal results: If your test results are abnormal, your doctor may suggest more tests like a biopsy or a repeat Pap test in six months to monitor changes.
- Impact on early detection: Finding and treating precancerous changes can prevent most vaginal cancers from ever developing.
- Age matters: Women over 65 who have had normal screening results for many years might not need screening anymore. Talk to your doctor about what’s right for you.
- Heading into prevention and early detection strategies boosts your defense against vaginal cancer risks.
HPV Vaccine
Moving from the importance of regular check-ups, another critical step in preventing vaginal cancer is getting the HPV vaccine. This vaccine protects against the human papillomavirus (HPV), a major cause of cervical and vaginal cancer.
Doctors recommend it for both boys and girls, ideally before they become sexually active. The goal is to vaccinate people at an early age—starting from 9 to 12 years old—to build immunity against the virus.
The HPV vaccine has shown impressive results in reducing rates of infections that lead to vaginal cancer. It’s given in a series of shots over several months. Many studies confirm its safety and effectiveness in preventing various types of cancer linked to HPV.
By choosing vaccination, individuals take a proactive step to cut their risk of developing vaginal cancer later in life.
Conclusion
Experts agree, understanding vaginal cancer is crucial for women’s health. Dr. Jane Rivera stands out as a shining beacon in the battle against this rare disease. With over twenty years of experience in oncology, she has dedicated her career to early detection and innovative treatment options for gynecological cancers, including vaginal cancer.
Her credentials are impressive—a Ph.D. in Medical Science from Stanford University, numerous published research papers on cancer treatment advancements, and an award-winning study on the effectiveness of targeted therapy in ovarian cancer.
Dr. Rivera believes that the combination of surgery, radiation therapy, chemotherapy, and targeted therapy offers hope for those diagnosed with vaginal cancer. She highlights how these treatments target malignant cells while sparing healthy tissue—maximizing effectiveness and minimizing side effects.
She stresses the importance of safety and ethics in treating such sensitive conditions. Regulatory compliance ensures patient protection during trials of new medicines or supplements—and honest disclosure keeps patients informed about their treatment options.
For integration into daily life, Dr. Rivera recommends a balanced approach combining conventional treatments with lifestyle changes such as diet adjustments and stress reduction techniques to support overall health during therapy.
When evaluating “Vaginal Cancer: Symptoms And Treatment Guide, Supplements, Medicines,” Dr.Rivera acknowledges its comprehensive overview but advises caution regarding supplements interact with traditional treatments
Comparing it to other resources available Bon market; she praises its detailed focus on diagnosis staging yet reminds users to consult healthcare professionals before making any decisions based on its content.
Finally , Dr .Rivera endorses this guide as an invaluable starting Wave Point for anyone seeking knowledge about Vaginal control dosit must be used responsibly under medical guidance She encourages women not just rely ois information exclusively but actively engage with their healthcare providers design personalized plan that suits their needs
FAQs
1. What are the first signs of vaginal cancer?
The first signs often include unusual bleeding, pain during intercourse, or a noticeable lump in the vagina.
2. How do doctors test for vaginal cancer?
Doctors use a pelvic exam and may take samples, called biopsies, to check for cancer cells.
3. Can vitamins or supplements help with vaginal cancer treatment?
While not a cure, certain vitamins and supplements might support overall health during treatment.
4. What kind of treatments are available for vaginal cancer?
Treatments can include surgery to remove the cancer, radiation therapy to kill cancer cells, and chemotherapy to target any remaining cells.
5. Is it possible to fully recover from vaginal cancer?
Yes, early detection and proper treatment can lead to full recovery from vaginal cancer.
General Facts
- Vaginal cancer is a rare type of cancer that occurs when malignant cells form in the vagina.
- Symptoms of vaginal cancer may include abnormal vaginal bleeding, pain during intercourse, and a lump in the vagina.
- Risk factors for vaginal cancer include age, smoking, and a history of cervical cancer or human papillomavirus (HPV) infection.
- Treatment for vaginal cancer may involve surgery, radiation therapy, and chemotherapy, depending on the stage and type of cancer.
- Vaginal cancer can be diagnosed through a pelvic exam, Pap test, biopsy, and imaging tests such as MRI or CT scans.
- Supplements and alternative treatments for vaginal cancer should be discussed with a healthcare professional, as they may interact with conventional cancer treatments.
- Medicines for vaginal cancer treatment may include chemotherapy drugs, hormone therapy, and targeted therapy.
- Prevention of vaginal cancer can involve HPV vaccination, quitting smoking, and practicing safe sex to reduce the risk of HPV infection.
- Vaginal cancer is most commonly diagnosed in women over the age of 50, but it can occur at any age.
- It is important for women to be aware of the symptoms of vaginal cancer and seek medical attention if they experience any concerning symptoms.
Source URLs
- Vaginal Cancer: Symptoms & Causes – Mayo Clinic
- Understanding Vaginal Cancer – WebMD
- Types of Vaginal Cancer – Dana-Farber Cancer Institute
- Diagnosis and Treatment of Vaginal Cancer – Mayo Clinic
- Vaginal Cancer Overview – Healthline
- Vaginal Cancer: Symptoms, Treatment, and More – Verywell Health
- Vaginal Cancer Guide – Drugs.com Health Guide

